A significant majority of adults in the United States remain largely unaware of a complex health condition, known as Cardiovascular-Kidney-Metabolic (CKM) syndrome, despite its pervasive influence, affecting an estimated 90% of the adult population. This recently defined health paradigm encompasses a constellation of serious ailments, including cardiovascular disease, chronic kidney disorders, diabetes, and obesity. A recent investigation conducted by the American Heart Association has illuminated a substantial deficit in public knowledge concerning CKM syndrome, yet concurrently revealed a strong desire among individuals to enhance their comprehension of this interconnected health issue.
The prevalence of risk factors associated with CKM syndrome is remarkably high, with nearly nine out of every ten American adults exhibiting at least one contributing element. These risk factors encompass elevated blood pressure, dysregulated cholesterol levels, persistently high blood glucose, excessive body weight, and diminished kidney function. When these individual challenges manifest concurrently, they synergistically amplify the likelihood of experiencing critical health events such as heart attacks, strokes, and heart failure to a degree far exceeding the sum of their isolated impacts. Encouragingly, for a considerable portion of affected individuals, the trajectory of CKM syndrome can be positively altered through deliberate lifestyle modifications, including dietary adjustments and increased physical activity, complemented by appropriate medical interventions.
Eduardo Sanchez, M.D., FAHA, chief medical officer for prevention at the American Heart Association, articulated a key objective: "We aim to foster a widespread understanding that experiencing simultaneous cardiovascular, renal, and metabolic risk factors is exceptionally common. It is heartening to note that once the CKM connection was formally delineated, nearly three-quarters of survey respondents recognized its significance and expressed a keen interest in learning more." This sentiment underscores a crucial point: the interconnectedness of these physiological systems, and the critical need for public awareness regarding their shared vulnerability.
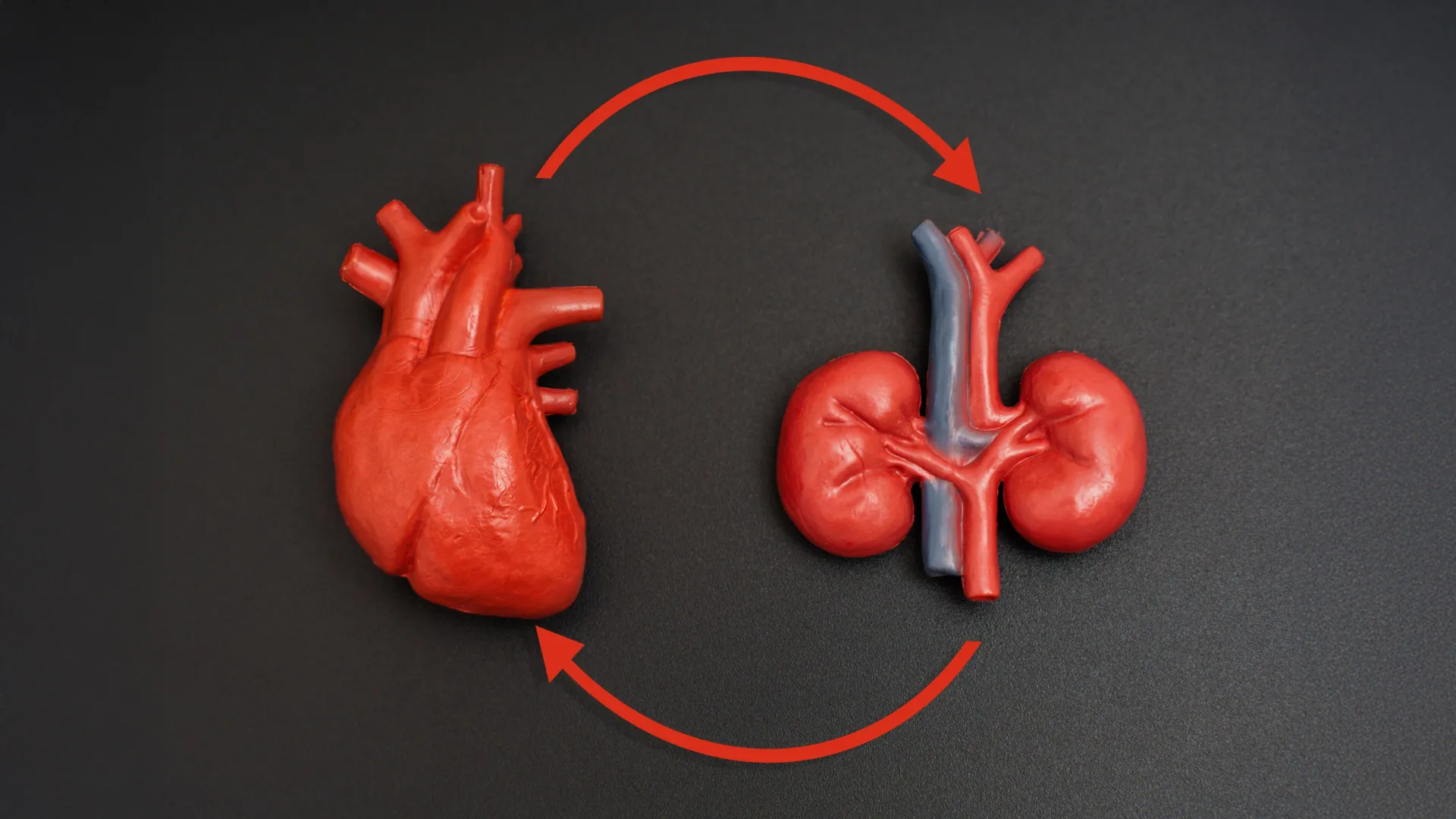
The intricate relationship between the heart, kidneys, and the body’s metabolic processes forms the bedrock of CKM health. The metabolic system, responsible for the intricate orchestration of energy production, utilization, and storage, directly influences weight regulation and blood glucose homeostasis. These vital organ systems function in a delicate interdependence; a compromise in one inevitably imposes additional strain on the others. This cascading effect, over time, can precipitate a detrimental feedback loop, markedly escalating the probability of developing CKM syndrome. In recognition of this growing public health concern, the American Heart Association is poised to introduce the inaugural clinical guidelines specifically addressing CKM syndrome in early 2026, a development anticipated to provide a crucial framework for diagnosis and management.
The aforementioned survey by the American Heart Association has starkly illuminated significant deficiencies in the public’s understanding of CKM health. Dr. Sanchez further emphasized the imperative of a holistic approach: "The cardiovascular, renal, and metabolic systems are intrinsically linked and, consequently, necessitate a coordinated approach to their management. The findings from this survey underscore the urgent need to highlight these interdependencies and empower patients to appreciate the value of collaborative care." This perspective highlights a critical gap in current healthcare paradigms, where these conditions are often managed in silos rather than as part of a unified health strategy.
In an effort to proactively address this knowledge deficit and empower individuals to take control of their well-being, the American Heart Association has launched its CKM Health Initiative. This initiative provides accessible educational resources and an online repository designed to elucidate the complex interrelationships between cardiovascular, renal, and metabolic health. The overarching goal is to equip individuals with the knowledge and tools necessary to implement proactive measures, thereby mitigating their risk of developing serious cardiovascular events such as heart attacks, heart failure, and strokes. Concurrently, the Association is actively engaged in fostering enhanced collaboration among healthcare professionals nationwide, aiming to cultivate a more integrated approach to the care of patients managing multiple chronic conditions.
A novel educational video, employing clear visuals and accessible language, offers a simplified framework for grasping CKM health by presenting "2 truths" about cardiovascular well-being. This multimedia approach aims to demystify complex physiological connections. "CKM health is fundamentally about your overall well-being," Dr. Sanchez stated. "It represents a complete cycle. By consistently monitoring your blood pressure, cholesterol levels, weight, blood sugar, and kidney function, you are actively contributing to your comprehensive health." This concise explanation underscores the actionable steps individuals can take to influence their CKM health.
The survey, commissioned by the American Heart Association and executed by The Harris Poll in August 2025, aimed to gauge public awareness levels regarding CKM syndrome and CKM health. The research involved the participation of approximately 4,000 adults across the United States. For healthcare professionals seeking further information on interdisciplinary care models and opportunities to engage with the CKM Health Initiative, resources are available at heart.org/CKMtools. The American Heart Association’s Cardiovascular-Kidney-Metabolic Health Initiative benefits from the foundational support of Founding Sponsors Novo Nordisk® and Boehringer Ingelheim, along with Supporting Sponsors Novartis Pharmaceuticals Corporation and Bayer, and Champion Sponsor DaVita®.
The research methodology employed for this study involved an online survey conducted within the United States by The Harris Poll on behalf of the American Heart Association. The sample comprised 4,007 U.S. adults aged 18 and older, with data collection occurring between August 6th and August 22nd, 2025. To ensure the findings accurately reflect the broader population demographics, the data were statistically weighted by factors including education level, age by gender, race/ethnicity, geographic region, household income, household size, marital status, employment status, and smoking habits. Participants were drawn from a pool of individuals who had voluntarily agreed to participate in online surveys. The margin of error for this study, measured using a Bayesian credible interval for Harris online polls, is estimated at plus or minus 2.0 percentage points at a 95% confidence level. It is important to acknowledge that the precision of the results may vary across different demographic subgroups. As with all survey research, potential sources of error, such as nonresponse bias, variations in question wording, and post-survey adjustments, may also be present.






