A newly elucidated molecular feedback loop has been identified as a critical driver of aggressive pancreatic cancer, offering a fresh perspective on therapeutic strategies for this formidable disease. Pancreatic ductal adenocarcinoma (PDAC), the predominant and most lethal form of pancreatic malignancy, has long presented a significant challenge to oncologists, with many patients developing resistance to current treatments, particularly those targeting the frequently mutated KRAS gene. This discovery, emerging from the laboratories at Cold Spring Harbor Laboratory (CSHL), points towards a complex interplay of proteins that fuels tumor progression, suggesting that disrupting this intricate circuit could be a promising avenue for future interventions.
The research builds upon prior work from 2023, which pinpointed the protein SRSF1 as an early instigator of PDAC tumor development. A deeper dive into the data from that initial study, conducted by a team led by former CSHL graduate student Alexander Kral, revealed that SRSF1 does not operate in isolation. Instead, it functions as a crucial component of a three-tiered molecular system that significantly enhances the cancer’s aggressiveness. "Our hypothesis was that some of the alterations induced by elevated SRSF1 levels were contributing to the observed rapid tumor growth," Kral articulated. "We focused our investigation on a molecule we suspected to be a major player, Aurora kinase A (AURKA). Our findings confirmed that it is integrated into a sophisticated regulatory pathway that encompasses not only AURKA and SRSF1 but also another critical oncogene, MYC."
This self-reinforcing cancer circuit operates through a series of interconnected molecular events. SRSF1 exerts its influence over AURKA by modifying the processing of its genetic instructions via a biological mechanism known as alternative splicing. This process results in an augmented abundance of AURKA. Subsequently, the elevated AURKA levels play a vital role in stabilizing and safeguarding the MYC protein. MYC, in turn, amplifies the production of SRSF1, thereby initiating the entire cascade once more and perpetuating the oncogenic loop that promotes cancerous growth. "While certain elements of this circuit were previously understood in isolation, the comprehensive picture remained elusive until this research," Professor Adrian Krainer, a senior researcher involved in the study, commented. "Once we established the involvement of AURKA’s alternative splicing, we could begin exploring methods to disrupt this critical pathway."
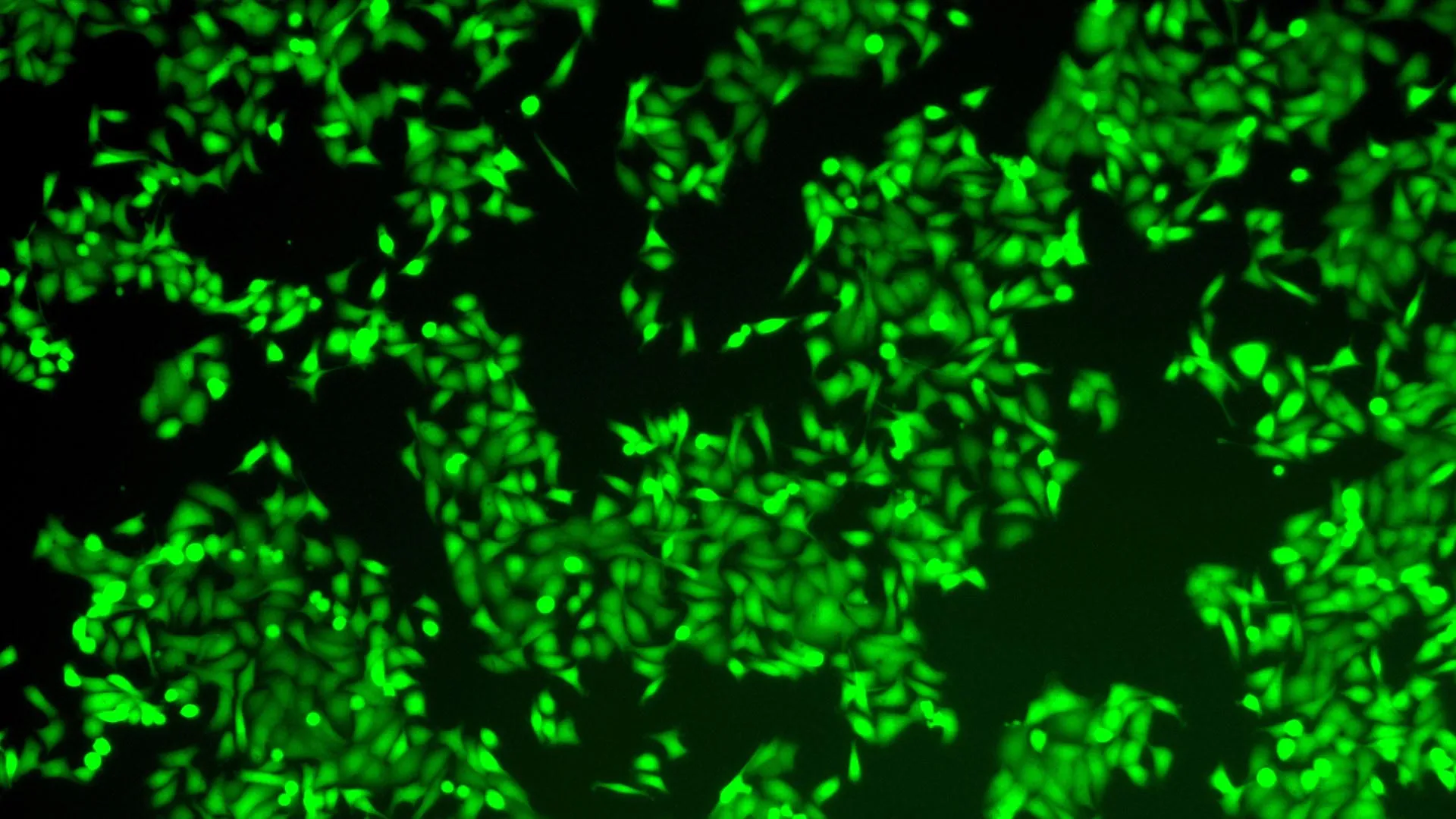
The potential to dismantle this cancer-driving mechanism lies in targeting a single key component. To achieve this, the research team engineered an antisense oligonucleotide (ASO). ASOs are short, synthetic molecules designed to interact with specific RNA sequences, thereby altering gene expression. The Krainer laboratory possesses extensive expertise in developing ASOs, notably having pioneered Spinraza, the first FDA-approved therapy for spinal muscular atrophy. Their initial expectation was that the newly developed ASO would specifically impede the alternative splicing of AURKA. However, when applied to pancreatic cancer cells, the effect proved to be far more profound than anticipated. The intervention caused the entire cancer-promoting circuit to collapse. Consequently, the tumor cells exhibited a marked loss of viability and initiated apoptosis, a programmed cell death pathway essential for maintaining tissue homeostasis.
"It’s akin to achieving multiple objectives with a single action," Professor Krainer elaborated. "SRSF1, AURKA, and MYC are all oncogenes that contribute to the progression of PDAC. By specifically targeting AURKA splicing with our ASO, we observed a simultaneous reduction in the levels of these other two key molecules." This observation underscores the interconnectedness of the identified circuit and highlights the potential for a single therapeutic intervention to exert a broad impact on tumor cell survival and proliferation.
The implications of this discovery for the future of pancreatic cancer therapy are significant. The Krainer lab is actively engaged in refining the ASO molecule, acknowledging that its clinical application in patients remains a long-term objective. Professor Krainer emphasizes the fundamental role of foundational research in driving medical breakthroughs, drawing a parallel to the development of Spinraza, which originated from basic scientific inquiry before transforming into a life-saving treatment for thousands. With continued development and optimization, this research holds the promise of contributing to the creation of novel and more effective therapeutic options for individuals battling pancreatic cancer. The identification of this specific molecular loop provides a concrete target for drug development, potentially circumventing the resistance mechanisms that have historically plagued PDAC treatment. Future research will likely focus on further characterizing the precise mechanisms by which this ASO induces apoptosis and loss of viability in cancer cells, as well as exploring its efficacy in preclinical models that more closely mimic the complex tumor microenvironment. Furthermore, understanding the broader applicability of this feedback loop to other cancer types could open up even more avenues for therapeutic innovation. The journey from laboratory discovery to patient bedside is often arduous and lengthy, but the unveiling of this intricate molecular circuitry represents a crucial step forward in the ongoing battle against one of the most challenging cancers known.






