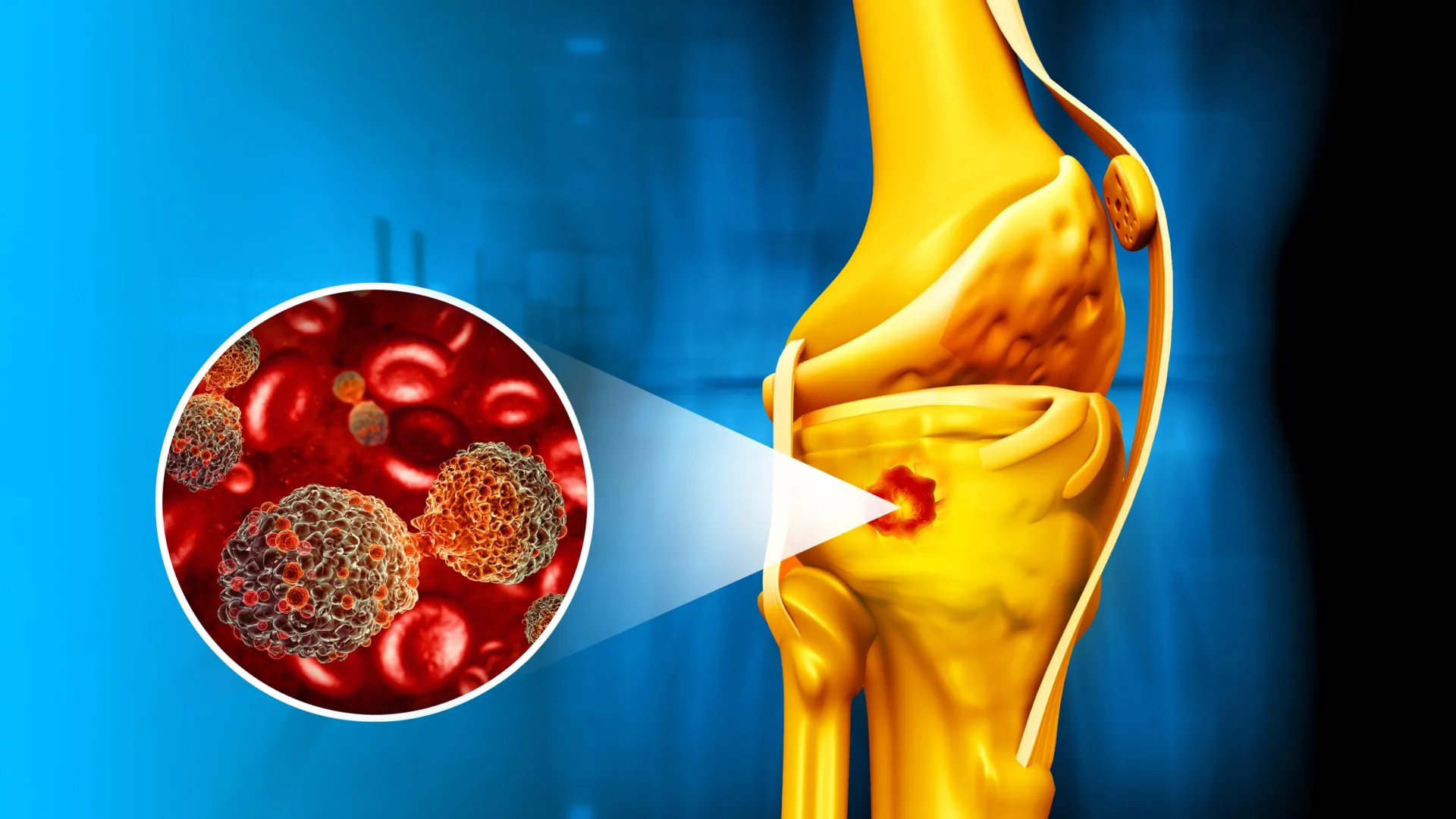
In a significant stride for oncological and regenerative medicine, a collaborative research endeavor between institutions in Brazil and Portugal has unveiled an innovative magnetic nanocomposite engineered to simultaneously combat malignant bone formations and facilitate the intricate process of skeletal repair. This groundbreaking material, detailed in a recent publication in Magnetic Medicine, represents a sophisticated answer to the complex challenges posed by bone cancers, particularly those requiring both aggressive therapeutic intervention and subsequent tissue reconstruction. The core innovation lies in its unique architectural design: a specialized core-shell configuration where highly efficient iron oxide nanoparticles are meticulously encapsulated within a delicate, yet robust, layer of bioactive glass. This thoughtful engineering endows the composite with a remarkable dual capability, allowing it to generate localized heat when exposed to an external magnetic field—a mechanism pivotal for targeted tumor destruction—while concurrently ensuring its steadfast integration with bone tissue and promoting cellular conditions conducive to natural bone regeneration.
The development of materials that seamlessly integrate such disparate, yet critically needed, functionalities has long represented a formidable hurdle within the field of biomedical engineering. Conventional approaches often necessitate separate interventions for tumor eradication and subsequent tissue repair, increasing procedural complexity, recovery times, and patient burden. The research team behind this novel material has meticulously addressed this challenge, converging magnetic hyperthermia capabilities, essential for precisely eliminating cancerous cells, with inherent properties that actively encourage the growth and remodeling of healthy bone tissue. This convergence into a single, cohesive material marks a pivotal advancement, promising a more streamlined and effective treatment paradigm for individuals afflicted with bone malignancies.
Dr. Ángela Andrade, the lead author of this seminal investigation, articulated the profound implications of these findings. "Magnetic bioactive nanocomposites hold immense promise for the treatment of bone cancer," Dr. Andrade explained, emphasizing their unprecedented capacity to "simultaneously ablate tumors through magnetic hyperthermia and actively support the formation of new bone." She further highlighted the scientific breakthrough achieved: "We have demonstrated the feasibility of achieving both robust magnetization within the nanocomposite and potent bioactivity within the same material, a dual characteristic that has eluded researchers for an extended period in this specialized domain." This statement underscores the material science triumph inherent in overcoming the often-conflicting requirements for magnetic performance and biological integration.
To rigorously evaluate the material’s potential efficacy and behavior within a physiological context, the research team conducted comprehensive in vitro studies. These experiments involved immersing the newly developed nanocomposites in a meticulously formulated simulated body fluid (SBF), a solution designed to mimic the ionic composition and pH of human physiological fluids. The observations were highly encouraging: under these simulated biological conditions, the nanoparticles rapidly initiated the formation of apatite. Apatite is a crucial mineral component that constitutes the primary inorganic matrix of natural bone, playing an indispensable role in its structural integrity and biological function. The swift deposition of this bone-like mineral provides compelling evidence of the material’s excellent osteoinductive properties and its strong propensity to chemically bond with existing bone tissue following implantation. This rapid mineralization suggests a high degree of biocompatibility and a strong potential for successful osseointegration, which is critical for long-term therapeutic success.
Further investigations involved a comparative analysis of several distinct formulations of the nanocomposite, each varying slightly in its precise chemical composition. This systematic approach allowed the researchers to fine-tune the material’s properties and identify optimal configurations. Among the various iterations examined, one particular variant, notably enriched with an elevated concentration of calcium, exhibited particularly outstanding performance across multiple key metrics. Dr. Andrade elaborated on this specific finding, stating, "Among the formulations evaluated, the one incorporating a higher calcium content distinguished itself by demonstrating both the most accelerated rate of mineralization and the most potent magnetic response." This superior performance, she concluded, positions this calcium-enriched composite as "an ideal candidate for a wide array of biomedical applications," especially those targeting bone health and regeneration. The enhanced calcium content likely contributes to a more robust and rapid apatite formation, while also potentially influencing the material’s magnetic characteristics in a beneficial way.
The fundamental principle underpinning the composite’s tumor-targeting capability lies within its iron oxide core. These magnetic nanoparticles, when subjected to an alternating magnetic field (AMF), possess the inherent ability to efficiently convert electromagnetic energy into thermal energy. This localized generation of heat, a process known as magnetic hyperthermia, can be precisely controlled to reach temperatures sufficient to induce irreparable damage or complete destruction of cancerous cells. Crucially, this method offers a significant advantage over systemic therapies, as the heat generation can be confined predominantly to the tumor site, thereby minimizing collateral damage to surrounding healthy tissues. This selective targeting is a cornerstone of modern cancer therapy, striving to maximize therapeutic efficacy while mitigating adverse side effects.
Concurrently, the specialized bioactive glass coating serves as an active catalyst for the healing process. Bioactive glasses are well-known for their unique ability to form a strong bond with bone by stimulating the deposition of apatite and encouraging the proliferation and differentiation of osteoblasts—the cells responsible for bone formation. By fostering a microenvironment conducive to regeneration, this outer layer actively promotes the restoration of damaged bone tissue. This synergistic action creates a holistic treatment strategy: the material not only addresses the immediate threat of tumor proliferation but also simultaneously initiates and supports the structural repair of the bone matrix. This integrated approach represents a paradigm shift, moving beyond mere tumor removal towards comprehensive functional restoration.
Dr. Andrade further elucidated the broader scientific contributions of their work, observing, "This investigation yields novel insights into the profound influence of surface chemistry and structural design on the overall performance characteristics of magnetic biomaterials." She emphasized that these discoveries "unveil new avenues for the development of increasingly sophisticated multifunctional materials that are demonstrably both safe and clinically effective." Understanding these intricate relationships between material design, surface properties, and biological interaction is paramount for advancing the next generation of therapeutic biomaterials.
In summation, this pioneering research represents a substantial leap forward in the burgeoning fields of smart nanomaterials for oncology and regenerative medicine. By successfully integrating robust magnetic performance, critical for targeted tumor ablation, with potent bone-friendly bioactivity, essential for tissue repair, these novel nanocomposites pave the way for future therapeutic modalities. Envisioned applications include treatments for bone tumors that could be delivered through a single, potentially minimally invasive procedure, offering the dual benefit of eradicating malignant cells and restoring compromised skeletal tissue. Such an integrated approach promises to significantly improve patient outcomes, reduce the burden of multi-stage treatments, and usher in an era of more sophisticated and patient-centric care for bone cancer and associated pathologies. The journey from laboratory discovery to widespread clinical application is often long and complex, requiring further in vivo studies, comprehensive safety assessments, and rigorous clinical trials. Nevertheless, this foundational research provides a compelling blueprint for the next generation of advanced medical interventions.






