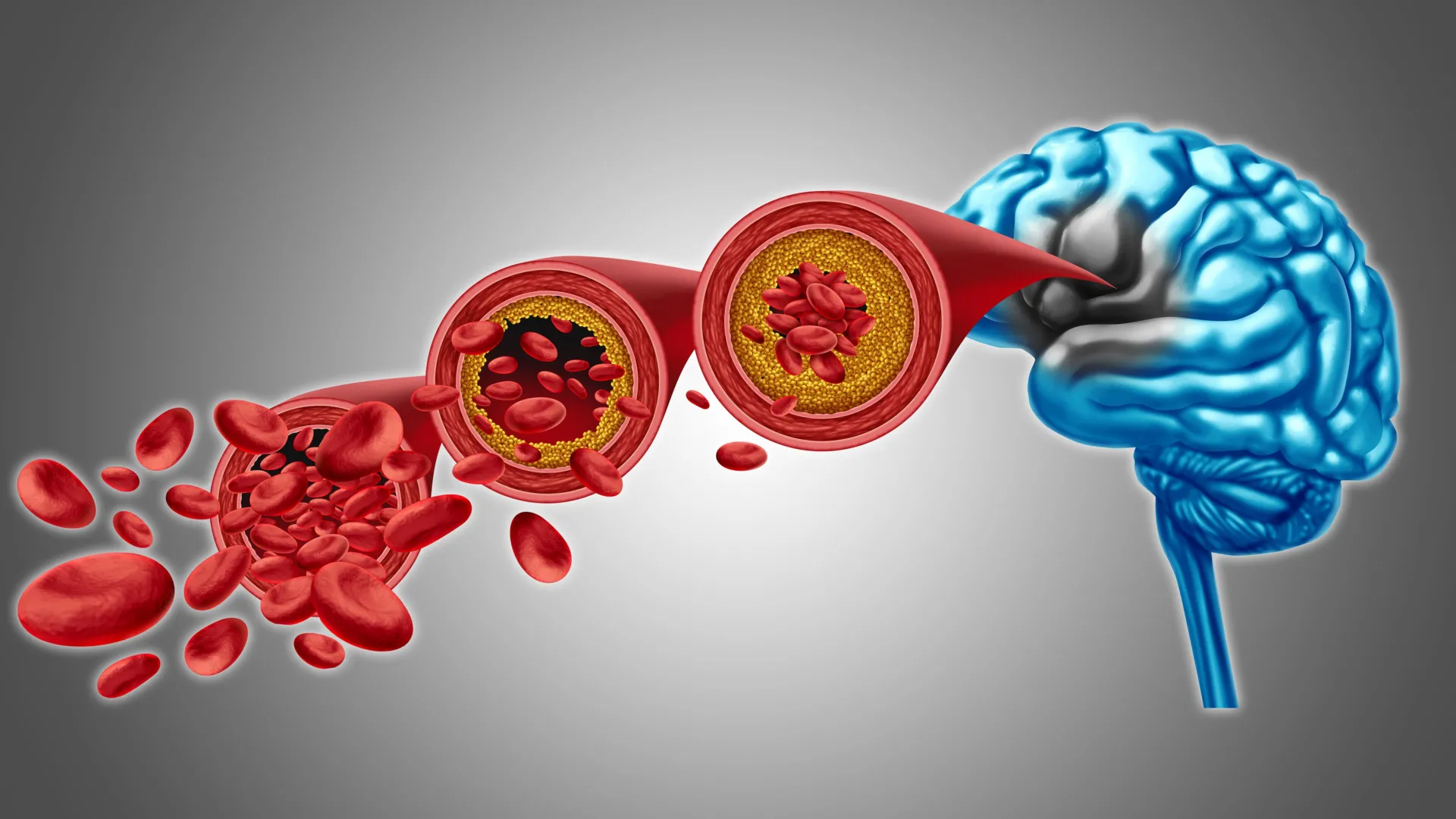
A significant advancement in understanding and potentially treating conditions characterized by diminished brain blood flow and certain forms of dementia has been reported by researchers at the University of Vermont Robert Larner, M.D. College of Medicine. Their preclinical investigations, detailed in the December 22nd edition of Proceedings of the National Academy of Sciences, illuminate crucial mechanisms governing cerebral blood flow and propose a novel therapeutic avenue involving the restoration of a specific lipid molecule. The findings suggest that replenishing a deficient phospholipid in the bloodstream could be instrumental in re-establishing healthy brain circulation and alleviating symptoms associated with neurodegenerative diseases.
Dr. Osama Harraz, an assistant professor of pharmacology and the principal investigator on this groundbreaking study, expressed optimism about the implications of their work. "This discovery represents a monumental stride in our collective endeavor to combat dementia and neurovascular ailments," Dr. Harraz stated. "We are progressively unraveling the intricate biological processes underlying these debilitating conditions, which now opens the door to conceptualizing tangible therapeutic interventions derived from this fundamental science."
The escalating global impact of Alzheimer’s disease and other dementia-related disorders is a growing concern, affecting an estimated 50 million individuals worldwide with projections indicating a continued rise. This increasing burden places immense strain on individuals, their families, caregivers, and the broader healthcare infrastructure. Ongoing scientific efforts are dedicated to dissecting the multifaceted contributions of protein dysregulation, inflammatory responses, aberrant neural signaling, and cellular dysfunction to the pathogenesis of these disorders.
The research conducted in Dr. Harraz’s laboratory specifically delves into the complex regulation of cerebral blood flow and the sophisticated communication pathways employed by blood vessels through molecular cues. A central element of their investigation revolves around Piezo1, a mechanosensitive protein embedded within the membranes of cells that form the inner lining of blood vessels. Piezo1 plays a critical role in modulating brain blood flow by detecting the physical forces generated by the pulsatile movement of blood through the brain’s intricate vascular network. The protein’s nomenclature is derived from the Greek word for "pressure," reflecting its sensitivity to mechanical stimuli. Previous research had already established that variations in the Piezo1 gene can lead to altered protein function in individuals.
The recent study, bearing the title "PIP2 Corrects an Endothelial Piezo1 Channelopathy," provides unprecedented clarity on how Piezo1 influences cerebral blood flow dynamics. Crucially, the findings establish a correlation between conditions such as Alzheimer’s disease and an overactive state of Piezo1 within the brain’s blood vessels. To elucidate the underlying causes of this dysregulation, the research team meticulously examined a vital phospholipid known as PIP2, which is a ubiquitous component of neuronal and glial cell membranes in the brain.
PIP2 performs indispensable functions in cellular signaling pathways and the intricate regulation of ion channels, a sophisticated biological mechanism that governs the precise opening and closing of protein pores within cell membranes. The researchers made a pivotal discovery: PIP2 naturally acts as a potent inhibitor of Piezo1 activity. Consequently, when the concentration of PIP2 declines, Piezo1 becomes excessively active, thereby disrupting the normal, regulated flow of blood within the brain. Conversely, when the research team introduced exogenous PIP2 into their experimental system, they observed a significant reduction in Piezo1 activity and a subsequent restoration of healthy blood circulation. These compelling results strongly indicate that augmenting PIP2 levels could serve as the foundational principle for a novel therapeutic strategy aimed at enhancing cerebral blood flow and bolstering overall brain function.
Looking ahead, future research endeavors will concentrate on precisely delineating the molecular interactions between PIP2 and Piezo1. Scientists aim to ascertain whether PIP2 directly binds to specific domains of the Piezo1 protein or whether it exerts its inhibitory effect by subtly altering the surrounding lipid environment of the cell membrane, thereby restricting the channel’s ability to open. Further investigations will also seek to unravel the precise mechanisms by which disease-associated reductions in PIP2 levels lead to the loss of this crucial regulatory control, allowing Piezo1 to persist in an overactive state and consequently impair cerebral blood flow. A comprehensive understanding of these fundamental biological processes will be paramount for the successful development of therapeutic interventions that either restore endogenous PIP2 levels or directly modulate Piezo1 activity to promote neurovascular health in the context of dementia and related vascular pathologies. This research holds promise for a new era of treatment for conditions previously considered intractable.