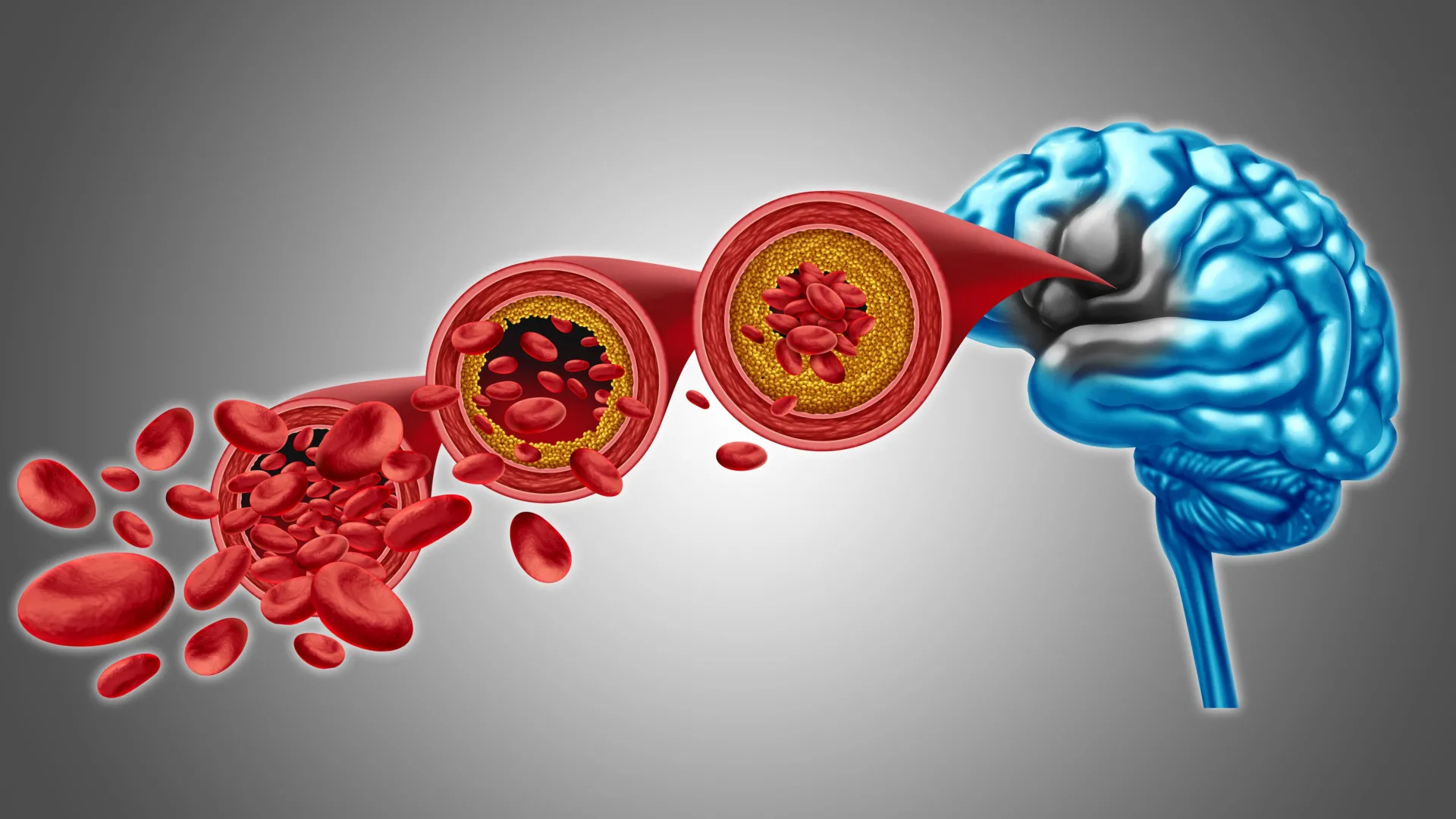
A groundbreaking preclinical investigation has illuminated a promising avenue for addressing the debilitating effects of compromised cerebral circulation, a condition intricately linked to various forms of dementia. Researchers at the University of Vermont’s Robert Larner, M.D. College of Medicine have meticulously detailed the intricate regulatory mechanisms governing blood flow within the brain, revealing a potential pathway to reverse vascular dysfunctions that contribute to cognitive impairment. Their findings, disseminated on December 22nd in the esteemed scientific journal Proceedings of the National Academy of Sciences, propose that the replenishment of a specific, deficient phospholipid within the bloodstream could serve to re-establish healthy brain blood flow and alleviate symptoms associated with dementia.
"This revelation represents a significant leap forward in our ongoing commitment to the prevention of dementia and neurovascular diseases," stated Dr. Osama Harraz, Ph.D., the principal investigator and an assistant professor of pharmacology at the Larner College of Medicine. "We are systematically unraveling the complex biological processes underlying these profoundly challenging conditions, and this newfound understanding positions us to conceptualize therapeutic interventions derived directly from this biological insight."
The escalating global impact of Alzheimer’s disease and its associated dementias is a pressing public health concern, currently affecting an estimated 50 million individuals worldwide, with projections indicating a continued rise in this figure. This burgeoning prevalence exerts considerable strain on familial support networks, professional caregivers, and the broader healthcare infrastructure. The scientific community is actively engaged in a multifaceted effort to decipher the contributions of various pathological elements, including protein misfolding, chronic inflammation, aberrant neural signaling, and cellular dysfunction, to the progression of these neurodegenerative disorders.
The research conducted within Dr. Harraz’s laboratory has centered on the sophisticated control of cerebral blood flow and the intricate communication pathways employed by blood vessels through molecular signaling. A pivotal element of their investigation has been Piezo1, a mechanosensitive ion channel protein embedded within the cellular membranes of the endothelium, the inner lining of blood vessels. Piezo1 plays a critical role in modulating brain blood flow by detecting the physical pressures generated by the dynamic movement of blood throughout the brain’s intricate vascular architecture. The protein’s nomenclature is derived from the Greek word for "pressure," underscoring its fundamental function. Previous research had already indicated that Piezo1 exhibits altered behavior in individuals possessing certain genetic variations affecting the Piezo1 gene.
The recently published study, bearing the title "PIP₂ Corrects an Endothelial Piezo1 Channelopathy," provides novel insights into the specific ways in which Piezo1 influences cerebral blood flow. Crucially, the research demonstrates a correlation between conditions such as Alzheimer’s disease and an overactive state of Piezo1 within the brain’s blood vessels. To thoroughly investigate the underlying causes of this hyperactivation, the research team turned their attention to a key phospholipid known as PIP₂ (phosphatidylinositol 4,5-bisphosphate), a molecule ubiquitously present in the membranes of brain cells.
PIP₂ performs an indispensable function in cellular communication and the precise regulation of ion channels, a complex biological process that governs the opening and closing of protein pores within cell membranes. The researchers’ groundbreaking discovery revealed that PIP₂ naturally acts as a potent inhibitory agent for Piezo1. Consequently, when the endogenous levels of PIP₂ decline, Piezo1 becomes excessively active, thereby disrupting the normal, regulated flow of blood within the brain. In a critical experimental demonstration, the introduction of exogenous PIP₂ into the affected biological system led to a significant reduction in Piezo1 activity and the subsequent restoration of healthy blood circulation. These findings strongly suggest that strategies aimed at augmenting PIP₂ levels could form the foundation of a novel therapeutic approach designed to enhance cerebral blood flow and bolster overall brain function.
The implications of these findings extend beyond the immediate discovery, paving the way for a series of crucial next steps in the development of future treatments. Ongoing and future research endeavors will be dedicated to precisely elucidating the molecular interactions between PIP₂ and Piezo1. Scientists aim to ascertain whether PIP₂ directly binds to specific functional sites on the Piezo1 protein or if it exerts its regulatory influence by subtly altering the biophysical properties of the surrounding cell membrane, thereby restricting the opening of the ion channel. Furthermore, additional investigations will explore the mechanisms by which disease-related decrements in PIP₂ levels disengage this vital regulatory control, permitting Piezo1 to remain in an overactive state and consequently impair cerebral blood flow. A comprehensive understanding of these intricate mechanisms will be paramount for the successful development of therapeutic interventions that either restore endogenous PIP₂ levels or directly modulate Piezo1 activity to improve neurovascular health in individuals afflicted with dementia and related vascular pathologies. This research offers a beacon of hope in the challenging fight against cognitive decline and the broader spectrum of neurovascular disorders.






