For over a century, the prevailing scientific consensus regarding Alzheimer’s disease (AD) has painted a grim picture: a degenerative process that, once initiated, is irreversible. This deeply entrenched perspective has largely channeled research efforts towards strategies focused on prevention or the deceleration of the disease’s relentless march, rather than on the ambitious goal of reclaiming cognitive faculties already compromised. Despite decades of intensive investigation and substantial financial investment, the landscape of Alzheimer’s therapeutics has seen no drug designed with the explicit objective of reversing cognitive decline and restoring lost brain function.
However, a groundbreaking study, meticulously conducted by a collaborative team from University Hospitals, Case Western Reserve University, and the Louis Stokes Cleveland VA Medical Center, is poised to fundamentally challenge this long-standing paradigm. Their research embarks on a daring inquiry: could brains exhibiting the advanced hallmarks of Alzheimer’s disease possess the capacity for recovery?
At the heart of this innovative research lies a novel focus on a critical biological failure: the disruption of the brain’s energy equilibrium. Published on December 22nd in the esteemed journal Cell Reports Medicine, the study, spearheaded by Dr. Kalyani Chaubey of the Pieper Laboratory, meticulously examined both human Alzheimer’s brain tissue and a variety of preclinical mouse models. Their findings pinpointed a significant deficit in the brain’s ability to sustain adequate levels of nicotinamide adenine dinucleotide (NAD+), a vital cellular energy molecule, as a primary driver of Alzheimer’s pathology. Crucially, the research demonstrated that maintaining a healthy balance of NAD+ not only conferred protection against the onset of the disease but also proved capable of reversing its effects in experimental settings.
The natural aging process is accompanied by a gradual decline in NAD+ levels throughout the body, including the brain. When these levels fall below a critical threshold, cellular functions essential for normal operation and survival become compromised. The researchers observed that this decline is markedly more pronounced in the brains of individuals afflicted with Alzheimer’s disease, a pattern that was consistently replicated in the genetically engineered mouse models used in the study.
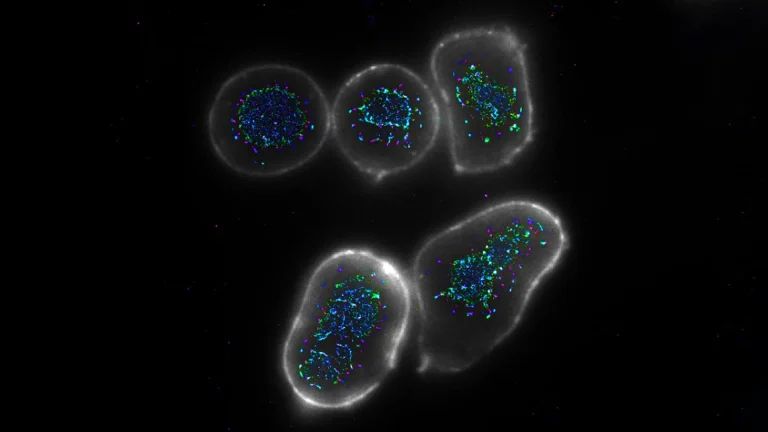
To accurately simulate the complexities of Alzheimer’s disease, which is exclusively a human affliction, scientists often employ specially developed mouse strains. These mice are engineered to carry specific human genetic mutations known to be causative agents of the disease in people. In this particular investigation, two distinct mouse models were utilized. The first group harbored multiple human gene mutations associated with amyloid processing, a key protein implicated in Alzheimer’s. The second group carried a human mutation within the tau protein, another protein central to the disease’s progression.
Abnormalities in amyloid and tau proteins represent some of the earliest and most significant pathological indicators of Alzheimer’s. In both mouse models, these genetic alterations precipitated widespread neurological damage that closely mirrored the pathological landscape observed in human Alzheimer’s brains. This included a breakdown of the blood-brain barrier, damage to neuronal axons, persistent neuroinflammation, a reduction in neurogenesis within the hippocampus (the brain region critical for memory formation), impaired communication between neurons, and extensive oxidative stress. Concurrently, these mice exhibited profound memory deficits and cognitive impairments analogous to those experienced by human patients.
Following the confirmation of significantly diminished NAD+ levels in both human and mouse Alzheimer’s brains, the research team set out to investigate two critical hypotheses. Firstly, they sought to determine whether preserving NAD+ balance prior to the manifestation of symptoms could confer preventative benefits. Secondly, and perhaps more remarkably, they aimed to ascertain if restoring this balance after the disease had already taken hold could lead to a reversal of existing damage.
This investigative approach was built upon the foundation of prior work from the same research group, published in the Proceedings of the National Academy of Sciences USA. That earlier research had established that the restoration of NAD+ balance could facilitate both structural and functional recovery following severe and prolonged traumatic brain injury. In the current study, the researchers employed P7C3-A20, a well-characterized pharmacological compound developed within the Pieper laboratory, as their tool to re-establish NAD+ homeostasis.
The experimental outcomes were nothing short of extraordinary. While maintaining NAD+ balance proved effective in preventing the development of Alzheimer’s pathology in the mice, the results observed when treatment commenced after the disease had already progressed to an advanced stage were even more astonishing. In these instances, the intervention aimed at restoring NAD+ balance enabled the brain to initiate repair mechanisms, effectively mending the significant pathological damage instigated by the genetic mutations.
Remarkably, both genetically distinct mouse models demonstrated a complete restoration of cognitive function. This functional recovery was corroborated by biochemical markers; blood tests revealed normalized levels of phosphorylated tau 217 (p-tau 217), a protein fragment that has recently gained approval as a crucial clinical biomarker for diagnosing Alzheimer’s in humans. These findings provided compelling evidence for disease reversal and simultaneously identified a promising biomarker for future human clinical trials.
The lead researchers expressed a sentiment of profound optimism, albeit tempered with scientific caution. Dr. Andrew A. Pieper, the senior author of the study and Director of the Brain Health Medicines Center at the Harrington Discovery Institute at University Hospitals, articulated his enthusiasm: "We were very excited and encouraged by our results." He elaborated, "Restoring the brain’s energy balance achieved pathological and functional recovery in both lines of mice with advanced Alzheimer’s. Seeing this effect in two very different animal models, each driven by different genetic causes, strengthens the idea that restoring the brain’s NAD+ balance might help patients recover from Alzheimer’s." Dr. Pieper holds significant academic positions, including the Morley-Mather Chair in Neuropsychiatry at UH and the CWRU Rebecca E. Barchas, MD, DLFAPA, University Professorship in Translational Psychiatry, and also serves as a Psychiatrist and Investigator at the Louis Stokes VA Geriatric Research Education and Clinical Center (GRECC).
These findings herald a potential paradigm shift in how Alzheimer’s disease is conceptualized and treated. "The key takeaway is a message of hope – the effects of Alzheimer’s disease may not be inevitably permanent," stated Dr. Pieper. "The damaged brain can, under some conditions, repair itself and regain function." Dr. Chaubey further emphasized the study’s contribution: "Through our study, we demonstrated one drug-based way to accomplish this in animal models, and also identified candidate proteins in the human AD brain that may relate to the ability to reverse AD."
It is imperative to differentiate this therapeutic strategy from the ingestion of over-the-counter NAD+-precursor supplements. Dr. Pieper cautioned against such conflation, noting that previous animal studies have indicated that these supplements can elevate NAD+ levels to potentially dangerous highs, a condition linked to increased cancer risk. The methodology employed in this research, conversely, utilizes P7C3-A20, a pharmacological agent specifically designed to assist cells in maintaining healthy NAD+ balance under conditions of extreme cellular stress, without pushing these levels beyond their normal physiological range. "This is important when considering patient care, and clinicians should consider the possibility that therapeutic strategies aimed at restoring brain energy balance might offer a path to disease recovery," Dr. Pieper advised.
This pioneering research not only offers a glimpse into potential Alzheimer’s reversal but also paves the way for subsequent investigations and, eventually, human clinical trials. The proprietary technology is currently undergoing commercialization by Glengary Brain Health, a Cleveland-based enterprise co-founded by Dr. Pieper. "This new therapeutic approach to recovery needs to be moved into carefully designed human clinical trials to determine whether the efficacy seen in animal models translates to human patients," Dr. Pieper explained. He outlined the next critical steps for the laboratory research: pinpointing the specific aspects of brain energy balance most crucial for recovery, identifying and evaluating complementary therapeutic avenues for Alzheimer’s reversal, and investigating the potential efficacy of this recovery approach in other forms of chronic, age-related neurodegenerative diseases.