A pivotal and comprehensive systematic review of existing research has definitively concluded that the use of acetaminophen, widely recognized by the brand name Tylenol, during pregnancy does not elevate the risk of developmental conditions such as autism spectrum disorder (ASD), attention-deficit hyperactivity disorder (ADHD), or intellectual disability in offspring. This significant scientific consensus, meticulously detailed in a January 16 publication within the esteemed journal The Lancet Obstetrics, Gynaecology & Women’s Health, represents the most extensive examination of the evidence to date, spearheaded by a dedicated team of investigators from City, University of London, in collaboration with St. George’s, University of London.
The impetus for this monumental undertaking was a resurgence of public apprehension, amplified by claims circulating in September 2025, which posited that prenatal exposure to acetaminophen could potentially disrupt fetal brain development and consequently increase the probability of a child developing autism. These concerns were not entirely without precedent, as earlier scientific investigations had identified subtle statistical correlations between maternal acetaminophen consumption during gestation and subsequent autism diagnoses in children. However, a critical examination of these prior studies revealed significant methodological shortcomings. Many were hampered by incomplete datasets, failed to adequately account for crucial confounding variables such as familial predisposition or genetic inheritance, and notably, lacked robust comparative analyses.
A substantial deficiency identified in previous research was the absence of head-to-head sibling comparisons, a methodology crucial for disentangling the influence of medication from inherited traits and shared environmental factors that invariably affect child development. To rigorously address these limitations and provide a more definitive answer, the current research consortium undertook a sophisticated systematic review and meta-analysis, synthesizing findings from an impressive 43 pre-existing studies. Their overarching objective was to definitively ascertain the safety profile of acetaminophen use during pregnancy.
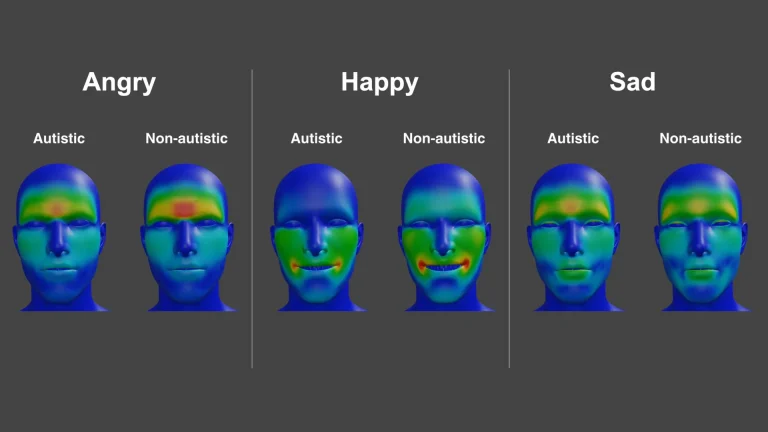
The researchers meticulously sifted through a vast body of evidence, prioritizing studies that offered the highest caliber of data. A cornerstone of their methodology involved direct comparisons between pregnancies where acetaminophen was administered and those where it was not. Of particular importance were studies that specifically analyzed siblings born to the same mother. Within this critical subgroup, researchers examined instances where one sibling had been exposed to acetaminophen in utero, while their sibling had not. This innovative approach offered a powerful means of controlling for a multitude of shared variables, including genetic backgrounds, the familial living environment, and persistent parental characteristics, all of which can exert a profound influence on a child’s developmental trajectory and are notoriously challenging to fully isolate in traditional observational studies.
The statistical power derived from these sibling comparison studies was substantial. The analysis encompassed developmental outcomes for an extensive cohort of 262,852 children assessed for autism, 335,255 evaluated for ADHD, and 406,681 assessed for intellectual disability. Across these expansive groups, the data revealed a resounding absence of any statistically significant evidence suggesting that maternal acetaminophen use during pregnancy was associated with an increased risk of developing any of these neurodevelopmental conditions, when contrasted with pregnancies where the medication was not utilized.
Professor Asma Khalil, a distinguished Professor of Obstetrics and Maternal Fetal Medicine at City, University of London, and a Consultant Obstetrician, who spearheaded this pivotal study, offered critical insights into why earlier research may have inadvertently generated apprehension. She explained, "Our findings strongly suggest that any previously reported associations are far more likely to be attributable to underlying genetic predispositions or other maternal health factors, such as fever or persistent pain, rather than a direct causative effect of paracetamol itself." Professor Khalil further emphasized the clear clinical message derived from this robust evidence, stating, "Paracetamol remains a safe and effective option during pregnancy when administered according to recommended guidelines. This is critically important, as paracetamol is the primary medication we advise for pregnant individuals experiencing pain or fever. Therefore, they can be confidently reassured that a safe and effective option is readily available to alleviate their symptoms."
The integrity of this comprehensive review was further bolstered by stringent quality control measures. Each of the 43 studies incorporated into the meta-analysis underwent rigorous evaluation utilizing the Quality In Prognosis Studies (QUIPS) tool. This standardized assessment framework meticulously examines multiple facets of study design to accurately gauge the potential for bias. Remarkably, the absence of any discernible link between prenatal acetaminophen exposure and the development of autism, ADHD, or intellectual disability remained consistently evident, even when the researchers narrowed their focus to include only those studies rated as having a low risk of bias, signifying the highest level of methodological rigor. Furthermore, these reassuring conclusions were replicated in studies that followed the children’s developmental progress for periods exceeding five years, lending further weight to the findings.
Despite the robust nature of the conclusions, the authors did acknowledge certain inherent limitations within the available body of research. Specifically, the existing data proved insufficient to conduct consistent examinations into whether potential risks might vary based on the trimester of pregnancy during which acetaminophen was used, the sex of the infant, or the frequency of medication administration. This was primarily due to a scarcity of detailed reporting on these specific parameters within the existing sibling comparison studies.
The implications of this extensive and meticulously conducted review are profound and far-reaching, aligning seamlessly with the established guidance issued by leading global medical organizations. The researchers express a strong hope that this thorough and authoritative analysis will effectively address and allay any persistent doubts or anxieties among pregnant individuals regarding the use of acetaminophen. It is well-established that untreated significant pain or fever during pregnancy can pose considerable risks to both the mother and the developing fetus. This compelling body of evidence unequivocally supports the continued and confident use of acetaminophen as a safe and appropriate therapeutic option when taken as directed, offering a vital means of symptom relief without introducing undue developmental concerns.