During an exceptionally severe influenza season, characterized by the pervasive circulation of a novel variant identified as subclade K, a recently unveiled investigation has yielded unexpected insights into the dynamics of viral dissemination and potential strategies for bolstering individual protection against infection. Researchers at the University of Maryland, spanning their Schools of Public Health and Engineering in College Park and the School of Medicine in Baltimore, devised a distinctive experimental protocol to meticulously observe the transmission pathways of the influenza virus. The study involved housing college students confirmed to be infected with influenza in a controlled hotel room environment alongside healthy middle-aged adult volunteers. Remarkably, despite prolonged and close interpersonal proximity, none of the healthy participants contracted the virus, a finding that challenges prevailing assumptions about the ease with which influenza spreads.
Dr. Donald Milton, a distinguished professor at the School of Public Health’s Department of Global, Environmental and Occupational Health and a recognized global authority in infectious disease aerobiology, who was instrumental in identifying methods to curb the spread of COVID-19, commented on the perplexing outcome. He stated, "At this juncture of the year, it appears as though nearly everyone is succumbing to the influenza virus. Yet, our study demonstrated a complete absence of transmission – what does this reveal about the mechanisms of flu propagation and effective strategies for outbreak containment?"
The investigation, officially published on January 7 in the esteemed journal PLOS Pathogens, marks a significant milestone as the first controlled clinical trial to rigorously examine airborne influenza transmission between individuals naturally infected with the virus, as opposed to those intentionally inoculated in a laboratory setting, and a cohort of uninfected subjects. Dr. Milton, alongside his colleague Dr. Jianyu Lai, a post-doctoral research scientist who spearheaded the data analysis and report compilation for the project, delved into several potential contributing factors that might explain the lack of observed transmission.
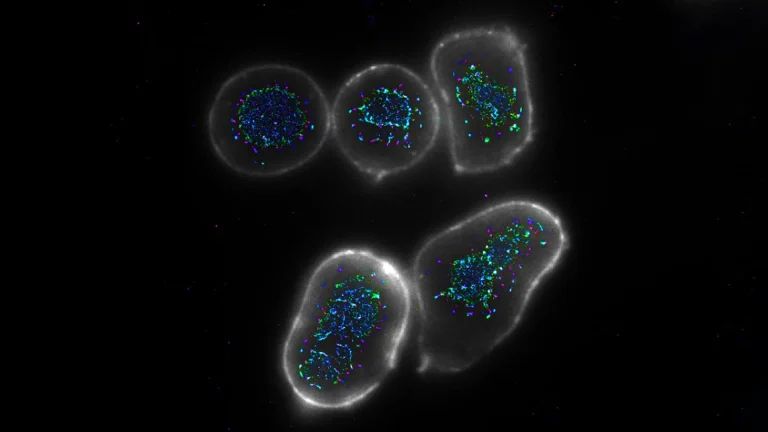
"Our data points towards critical elements that significantly influence the probability of flu transmission – coughing emerges as a primary factor," explained Dr. Lai. Although the infected student participants exhibited substantial viral loads within their nasal passages, Dr. Lai noted that instances of coughing were infrequent. Consequently, the quantity of viral particles released into the ambient air was considerably limited.
Furthermore, the study underscored the pivotal role of ventilation. "Another crucial determinant is ventilation and the circulation of air. The atmosphere within our experimental room was continuously and vigorously mixed by a heating and dehumidifying apparatus, which effectively diluted the minimal viral particles present in the air," Dr. Lai elaborated. The age demographic of the participants also emerged as a potential protective element. According to Dr. Lai, middle-aged adults generally exhibit a lower susceptibility to influenza compared to younger adults, a factor that likely contributed to the absence of infections within this group.
The implications of this research for influenza prevention are substantial. While a broad scientific consensus posits that airborne transmission is a principal driver of flu dissemination, Dr. Milton emphasized the necessity of robust evidence derived from randomized clinical trials, such as the one conducted, to substantiate changes in global infection-control guidelines. The research consortium is continuing its endeavors to gain a more profound understanding of how influenza propagates through inhalation and the specific environmental conditions that maximize transmission risk. The observed lack of transmission in this particular study offers invaluable insights into actionable measures individuals can implement to mitigate their personal risk during flu season.
"Being in close proximity, face-to-face with other individuals in indoor settings where air movement is minimal appears to represent the highest-risk scenario – and it is precisely this behavior that we tend to engage in frequently," Dr. Milton observed. "Our findings suggest that portable air purifiers designed to enhance air circulation while simultaneously filtering it could offer significant benefits. However, if one finds themselves in very close proximity to someone who is coughing, the most effective safeguard remains the use of a mask, particularly an N95 respirator."
The experimental phase of this influenza research was conducted on a sequestered floor of a hotel in the Baltimore metropolitan area, involving five participants who presented with confirmed influenza symptoms and eleven healthy volunteers. The study was executed in two distinct phases during the 2023 and 2024 periods. A comparable quarantine methodology had been employed in prior research initiatives, augmented by specialized exhaled breath analysis techniques developed by Dr. Milton and his associates. Participants resided on the isolated hotel floor for a fortnight, adhering to daily routines meticulously designed to simulate typical social interactions. These activities encompassed informal conversations and physical engagements such as yoga, stretching exercises, and dancing. Infected participants also interacted with shared objects, including a pen, a tablet computer, and a microphone, which were subsequently circulated among the group. Researchers diligently monitored participants for the onset of symptoms and collected daily nasal swabs, saliva samples, and blood samples to track viral load and antibody development. They quantified viral exposure both within the air breathed by participants and in the general room environment. Exhaled breath samples were systematically collected on a daily basis utilizing the Gesundheit II device, an apparatus conceptualized and developed by Dr. Milton and his collaborators at the Harvard T.H. Chan School of Public Health.
The ongoing pursuit of enhanced influenza outbreak mitigation strategies remains a paramount public health objective, according to Dr. Milton. Influenza continues to impose a considerable burden on healthcare systems globally. Annually, an estimated one billion individuals worldwide contract seasonal influenza. Within the United States alone, the current season has already recorded a minimum of 7.5 million cases, resulting in 81,000 hospitalizations and exceeding 3,000 fatalities. The research team comprised contributions from a multidisciplinary group of researchers affiliated with UMD’s Public Health Aerobiology Lab, including Kristen Coleman, Yi Esparza, Filbert Hong, Isabel Sierra Maldonado, Kathleen McPhaul, and S.H. Sheldon Tai. Additional collaborators hailed from the UMD Department of Mechanical Engineering, the University of Maryland School of Medicine, the Icahn School of Medicine at Mount Sinai in New York, the University of Hong Kong, and the University of Michigan, Ann Arbor. Financial support for this research was provided through the NIAID Cooperative agreement U19 grant (5U19AI162130), the University of Maryland Baltimore Institute for Clinical and Translational Research (ICTR), the University of Maryland Strategic Partnership: MPowering the State (MPower), and generous contributions from The Flu Lab and the Balvi Filantropic Fund.