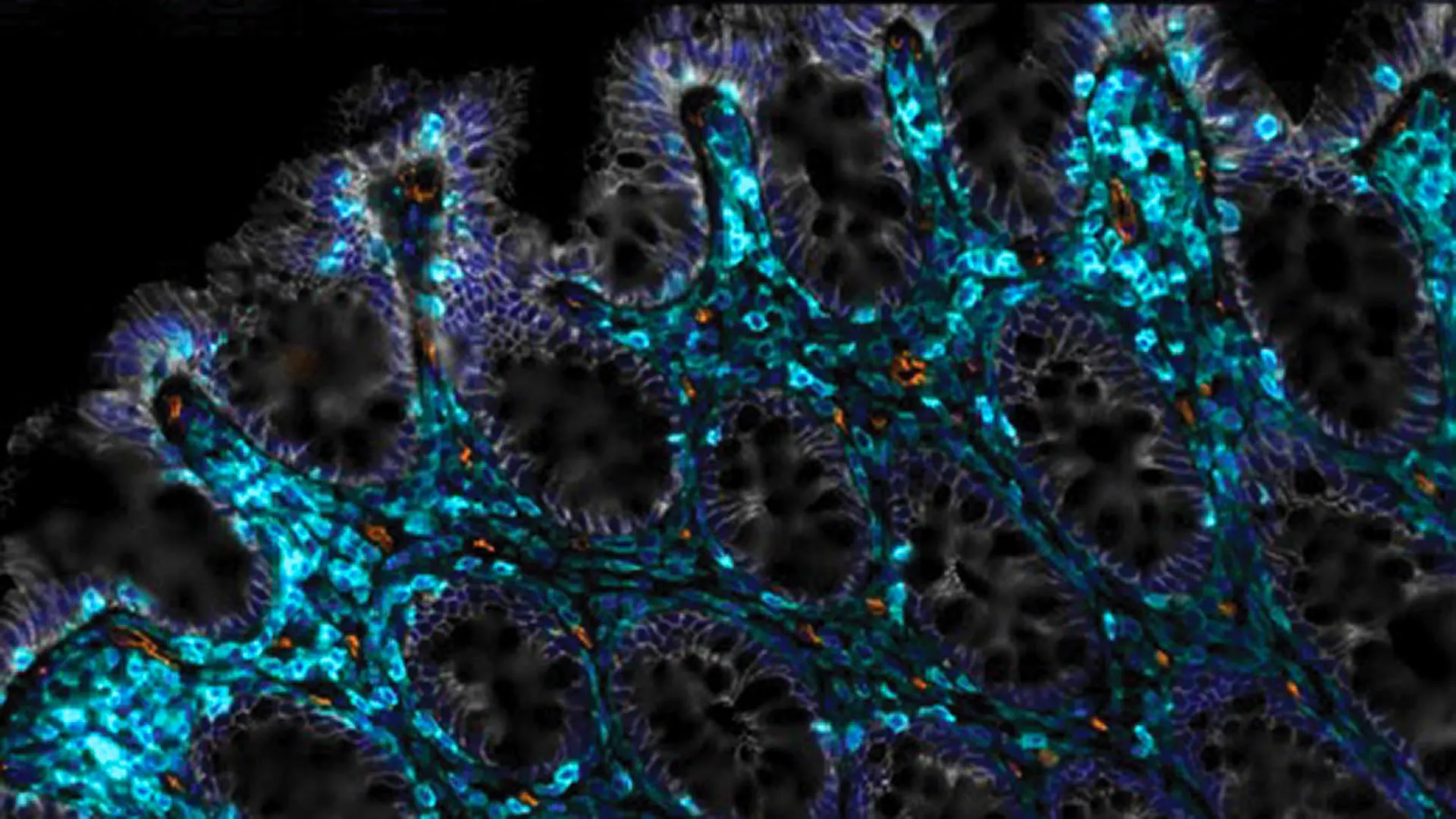
As individuals advance in age, many report a growing intolerance to certain foods and a general decline in digestive comfort. This common experience is often rooted in the gradual deterioration of the intestinal epithelium, a critical single layer of cells that forms the inner lining of the gut. This delicate barrier is indispensable for the proper absorption of nutrients and acts as a crucial defense against harmful substances. Under optimal conditions, the intestinal lining exhibits remarkable regenerative capabilities, completely renewing itself approximately every three to five days. However, this vital process can be severely compromised by the passage of time, age-related cellular changes, or aggressive medical interventions such as cancer radiation therapy. When this self-renewal mechanism falters or ceases entirely, it can trigger chronic inflammation, diminish the gut’s ability to absorb essential nutrients, and pave the way for debilitating conditions like "leaky gut syndrome," where the compromised barrier allows toxins and undigested food particles to enter the bloodstream.
In a significant stride toward addressing these age-related and damage-induced gastrointestinal challenges, scientists at Cold Spring Harbor Laboratory (CSHL) have uncovered a novel and highly promising method to reactivate the gut’s intrinsic repair systems. Their innovative approach repurposes a powerful form of immunotherapy, known as CAR T-cell therapy, which has primarily gained recognition for its efficacy in treating specific types of cancer. By ingeniously adapting this cutting-edge therapeutic strategy to the context of intestinal health, the research team aims to accelerate the pathway toward future clinical investigations. These trials would seek to dramatically improve the digestive well-being of individuals most affected by the natural decline associated with aging and those recovering from medical treatments that impact gut integrity.
Central to this groundbreaking research is the concept of cellular senescence, a biological phenomenon where cells cease to divide but paradoxically resist programmed cell death, or apoptosis. Often referred to as "zombie cells," senescent cells accumulate in tissues throughout the body as organisms age. While they no longer contribute to tissue growth or repair, they remain metabolically active, secreting a potent cocktail of inflammatory molecules, proteases, and growth factors known as the Senescence-Associated Secretory Phenotype (SASP). This persistent inflammatory milieu and tissue-disrupting activity are strongly implicated in the pathogenesis of numerous age-related diseases, ranging from metabolic disorders like diabetes to neurodegenerative conditions such as dementia. Therefore, the strategic removal of these lingering, non-functional cells represents a compelling target for interventions aimed at mitigating the multifaceted effects of aging.
This latest work builds upon a foundational body of research spearheaded by CSHL Assistant Professor Corina Amor Vegas, whose laboratory is dedicated to understanding the intricate mechanisms of cellular senescence. In previous pioneering studies, Dr. Amor Vegas and her team successfully engineered specialized immune cells—specifically, anti-uPAR CAR T cells—designed to precisely identify and eliminate senescent cells in laboratory mice. The outcomes of these earlier experiments were highly encouraging, demonstrating substantial improvements in the animals’ metabolic health following the targeted clearance of senescent cells. This prior success established a strong rationale for exploring whether a similar approach could be leveraged to restore the regenerative capacity of other vital tissues, particularly those with high turnover rates like the intestinal lining.
Driven by this hypothesis, the researchers extended their investigation to ascertain whether the selective removal of senescent cells could indeed enhance the intestine’s innate ability to heal itself. Dr. Amor Vegas initiated a collaborative effort with CSHL Assistant Professor Semir Beyaz and graduate student Onur Eskiocak to delve into this question. Their experimental design involved directly administering the specially engineered CAR T cells into the intestines of both younger and older mouse models. The results, as described by Dr. Amor Vegas, were nothing short of remarkable. She noted, "In both scenarios, we observed truly profound improvements." These benefits manifested as a significantly enhanced capacity for nutrient absorption, a marked reduction in intestinal inflammation, and, crucially, a much faster rate of regeneration and healing in the epithelial lining following induced irritation or injury. This demonstrated that by clearing senescent cells, the gut’s microenvironment became conducive to robust repair, irrespective of the animal’s chronological age.
The implications of these findings extend particularly to vulnerable populations, such as cancer patients undergoing radiation therapy. Leaky gut syndrome and severe gastrointestinal distress are notoriously common side effects among individuals receiving pelvic or abdominal radiation, which can inflict extensive damage on the rapidly dividing intestinal epithelial cells. To meticulously model this clinical scenario, the research team exposed mice to controlled doses of radiation designed to injure their intestinal epithelial cells. The subsequent recovery observed in mice that received the CAR T-cell treatment was dramatically more effective and complete compared to their counterparts who did not receive the therapeutic intervention. A particularly noteworthy discovery was the enduring protective effect of the therapy: a single dose of the CAR T-cell treatment continued to support healthier gut function and resilience for an impressive duration of at least one year, suggesting a durable reset of the intestinal regenerative machinery.
Further bolstering the therapeutic potential of this approach, the researchers gathered compelling evidence indicating that anti-uPAR CAR T cells also actively promote regeneration in human intestinal and colorectal cells grown in laboratory settings, as highlighted by Eskiocak. While the precise and intricate biological mechanisms underpinning this regenerative effect are still undergoing thorough exploration and elucidation, the consistent and robust nature of the findings strongly points toward significant therapeutic promise. Dr. Beyaz underscored the broader philosophical and practical importance of this work, remarking, "This represents a crucial advancement in our extensive quest to deepen our understanding of how we can more effectively facilitate healing and recovery in elderly populations." This perspective positions the research not merely as a gut-specific solution but as a foundational step in a wider effort to combat age-related decline at a cellular level.
The far-reaching implications of this research are profound. Beyond directly addressing the specific challenges of age-related digestive decline and radiation-induced gut damage, the success of targeted senescent cell removal in promoting tissue regeneration opens new avenues for treating a multitude of conditions associated with aging. By demonstrating that the gut’s healing capacity can be rejuvenated through the selective elimination of these detrimental "zombie cells," the CSHL team has illuminated a potential paradigm shift in regenerative medicine. Future research will undoubtedly focus on refining the CAR T-cell therapy for human application, meticulously exploring its long-term safety and efficacy, and investigating its potential utility in other organs and tissues burdened by cellular senescence. The prospect of clinical trials now appears significantly closer, offering hope for enhanced quality of life for an aging global population and for cancer survivors grappling with the debilitating aftermath of life-saving treatments. This innovative strategy marks a significant step towards unlocking the body’s latent regenerative potential, signaling a new era in the fight against age-related degeneration and chronic disease.






