The intricate ecosystem within the human mouth, a bustling metropolis of microorganisms, plays a pivotal role in maintaining oral health or, conversely, in initiating destructive processes like tooth decay. At the heart of this dynamic environment are bacteria that, when presented with dietary sugars, engage in a metabolic dance that results in the liberation of acidic byproducts. These acids, over time, possess the formidable capacity to demineralize and ultimately erode the protective outer layer of teeth, known as enamel, paving the way for the development of cavities. The pathogenic bacteria responsible for this assault do not operate in isolation; instead, they coalesce and construct complex, adherent structures colloquially termed dental biofilms. These biofilms, often appearing as plaque, serve as tenacious shields that anchor bacteria to tooth surfaces, creating microenvironments where acid production can be amplified, thus accelerating the rate of tooth damage.
Within this microbial community, a naturally occurring amino acid, arginine, has emerged as a significant player in the ongoing battle against dental caries. Scientific inquiry has illuminated the crucial role of arginine in mitigating the detrimental effects of acid production. Certain beneficial bacterial species are equipped with a specialized metabolic pathway, the arginine deiminase system (ADS), which enables them to convert arginine into alkaline compounds. These alkaline substances act as natural buffers, effectively neutralizing the harmful acids generated by other bacteria. The prevailing hypothesis is that an increased availability of arginine fosters the proliferation of these protective, acid-neutralizing bacteria, while simultaneously hindering the growth and acid-producing capabilities of cariogenic (cavity-causing) bacteria. Prior investigations, conducted in controlled laboratory settings, had already hinted at arginine’s capacity to modulate the overall composition and structure of dental biofilms.
To ascertain whether these promising laboratory observations translate to tangible benefits within the complex milieu of a living human mouth, a dedicated research initiative was undertaken by a team of scientists at Aarhus University in Denmark. Spearheaded by Postdoctoral Fellow Yumi C. Del Rey and Professor Sebastian Schlafer from the Department of Dentistry and Oral Health, this clinical study aimed to provide empirical evidence for arginine’s anticaries potential. The findings of their rigorous investigation were subsequently disseminated in the esteemed scientific journal, the International Journal of Oral Science.
The study’s methodology involved a cohort of twelve participants who were experiencing active tooth decay, a condition characterized by the presence of ongoing carious lesions. To facilitate precise sampling and controlled exposure, each participant was fitted with specially engineered dentures. These bespoke devices were designed to enable the researchers to meticulously collect intact dental biofilms from distinct regions within both sides of the oral cavity. Participants engaged in a standardized protocol: they were instructed to immerse their dentures in a sugar-containing solution for a duration of five minutes. Immediately following this sugar exposure, one side of the mouth received an application of distilled water, serving as a placebo control, while the contralateral side was treated with an arginine solution. This carefully orchestrated regimen was administered three times daily, with the arginine treatment consistently applied to the same designated side of the mouth throughout the study period.
Professor Sebastian Schlafer articulated the precise objectives of their research, stating, "The aim was to investigate the impact of arginine treatment on the acidity, type of bacteria, and the carbohydrate matrix of biofilms from patients with active caries." This comprehensive approach allowed the researchers to examine multiple facets of biofilm behavior under the influence of arginine. Following a four-day period, during which the biofilms were allowed to fully mature and develop on the dentures, the prosthetics were carefully removed for in-depth analysis.
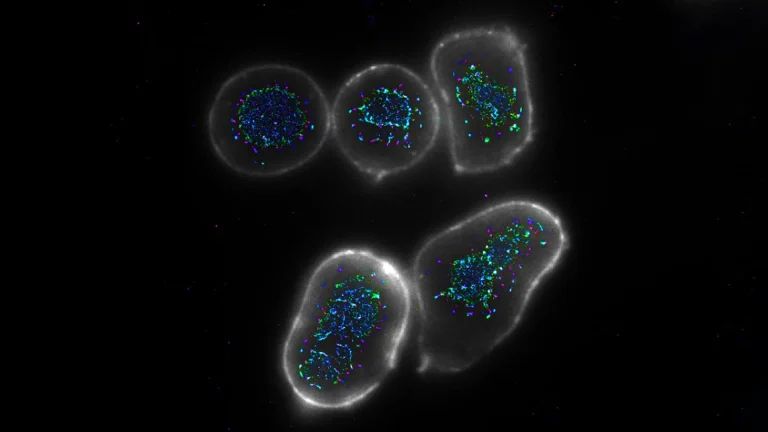
A critical aspect of the investigation involved quantifying the acidity within the dental biofilms. To achieve this, the researchers employed a sophisticated pH-sensitive dye known as "C-SNARF-4." This fluorescent dye provided a nuanced method for assessing the acid levels across different microdomains within the biofilm structure. The data unequivocally demonstrated a significant difference: biofilms that had been subjected to arginine treatment exhibited markedly higher pH values—indicating reduced acidity—at both the 10-minute and 35-minute marks subsequent to exposure to the sugar solution.
Yumi C. Del Rey, the lead author of the study, underscored the significance of these findings, remarking, "Our results revealed differences in acidity of the biofilms, with the ones treated with arginine being significantly more protected against acidification caused by sugar metabolism." This observation directly supports the notion that arginine actively counteracts the acidogenic challenge posed by dietary sugars.
Beyond acidity, the research team delved into the structural intricacies of the biofilms and their constituent carbohydrate components. They utilized fluorescently labeled lectins, which are proteins with a remarkable affinity for specific carbohydrate molecules, to probe these structural elements. Two principal carbohydrate components of particular interest were fucose and galactose. These sugars are known to constitute a substantial proportion of dental biofilms and are implicated in the formation of localized "acidic pockets" that can trap and concentrate destructive acids in close proximity to tooth surfaces.
The analysis revealed a compelling shift in biofilms exposed to arginine: there was a discernible reduction in the abundance of fucose-based carbohydrates. This decrease in fucose may contribute to a diminished capacity of the biofilm to foster harmful acidic conditions. Furthermore, the researchers observed a notable alteration in the spatial organization of galactose-containing carbohydrates. These sugar molecules, which were previously more evenly distributed, became less prevalent near the base of the biofilm and showed increased concentration towards the apical (top) surface. This reorganization suggests a potential mechanism whereby arginine influences the biofilm’s architecture to limit the accumulation of acids near the critical tooth surfaces.
A fundamental component of understanding oral health is characterizing the microbial inhabitants of the mouth. To this end, the researchers employed a powerful molecular technique, "16S rRNA gene sequencing," to analyze the bacterial DNA present in the biofilms. This method allowed for the precise identification and quantification of different bacterial species. The findings indicated that biofilms treated with either arginine or the placebo were predominantly populated by Streptococcus and Veillonella species. However, a significant divergence emerged with arginine treatment: there was a marked reduction in the prevalence of the mitis/oralis group of streptococci. This particular subgroup of streptococci is known for its acid-producing capabilities but possesses a relatively weak capacity for generating alkaline substances.
Concurrently, the study noted a modest increase in the proportion of streptococci species that exhibit a greater proficiency in metabolizing arginine. This subtle but significant shift in the microbial community composition appears to be a key driver in elevating the intra-biofilm pH levels. Collectively, these findings paint a clear picture: arginine actively contributes to rendering dental biofilms less detrimental by lowering acidity, modifying their carbohydrate composition, and reshaping the resident microbial community towards a more benign profile.
Given the widespread prevalence of tooth decay across all age demographics globally, the implications of this research are substantial. The researchers propose that the strategic incorporation of arginine into commonly used oral hygiene products, such as toothpastes and mouthwashes, could represent a safe and highly effective prophylactic strategy. This approach holds particular promise for individuals who are disproportionately susceptible to developing cavities. Moreover, considering that arginine is an amino acid naturally synthesized by the human body and is a common constituent of numerous dietary proteins, its inclusion in oral care formulations is deemed safe. This inherent safety profile suggests that arginine-based oral hygiene products could potentially be suitable for use even in pediatric populations.