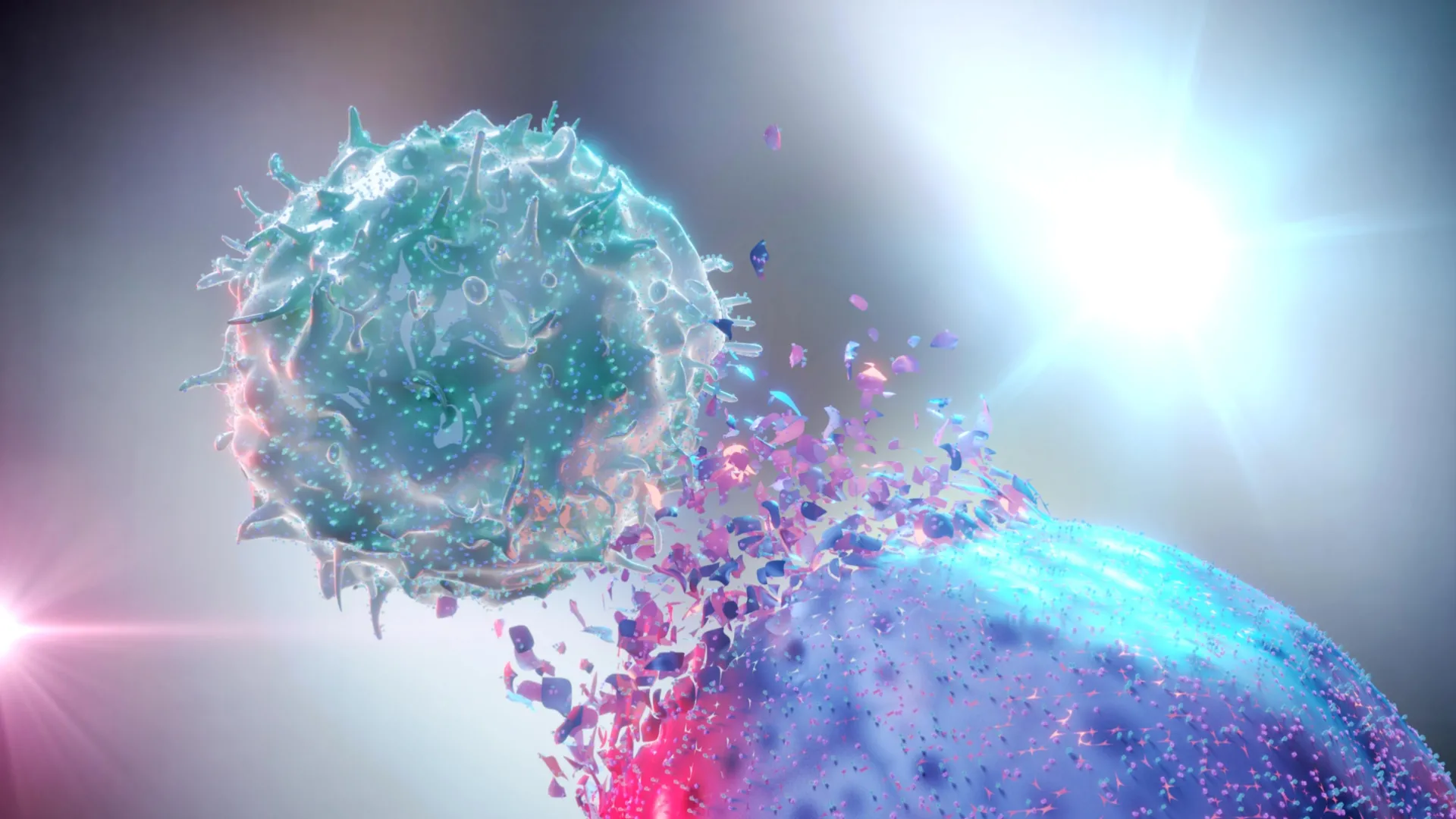
Natural killer (NK) cells stand as frontline sentinels within the body’s intricate defense network, playing a crucial role in maintaining health by identifying and neutralizing threats. These specialized immune cells are instrumental in combating invading pathogens, clearing cellular debris, and eliminating cells that have become compromised by infection or have undergone malignant transformation. Their vigilant patrol extends throughout the circulatory system and into various tissues, where they act swiftly to prevent the proliferation of harmful agents. A depletion in the population or functional capacity of these NK cells can significantly impair the immune system’s ability to fend off disease, leaving the body more susceptible to illness.
Recent scientific inquiry has delved into the intricate relationship between common psychological conditions, namely anxiety disorders and insomnia, and their potential impact on the levels of these vital immune cells. Recognizing the escalating prevalence of both anxiety and sleep disturbances, a research team based in Saudi Arabia undertook a comprehensive investigation to explore these connections. Their findings, recently published in the esteemed journal Frontiers in Immunology, shed light on how these states of psychological distress may compromise the body’s natural defenses, specifically by reducing the numbers of NK cells.
The study’s lead author, Dr. Renad Alhamawi, an assistant professor of immunology and immunotherapy at Taibah University, articulated the significance of their discoveries, stating, "We observed a notable reduction in both the overall count and the proportion of total NK cells, as well as their distinct sub-populations, among students experiencing symptoms of insomnia." She further elaborated on the findings related to anxiety, noting, "Conversely, individuals reporting general anxiety symptoms exhibited a diminished percentage and absolute number of circulating NK cells and their associated subtypes when compared to their peers who were symptom-free." This suggests a differential, yet equally detrimental, impact of these psychological states on the immune system.
The research methodology involved a cohort of 60 female students, aged between 17 and 23 years, who voluntarily participated in the study. Each participant was meticulously assessed using a battery of three standardized questionnaires. These instruments were designed to gather sociodemographic information and to comprehensively evaluate the presence and severity of symptoms related to both anxiety and insomnia. The reporting of anxiety and sleep disturbances was based on the participants’ self-assessment, providing a subjective yet critical measure of their psychological well-being. The survey data revealed a significant prevalence of these conditions within the student population: approximately 53 percent of the participants reported experiencing sleep difficulties consistent with the diagnostic criteria for insomnia, while a substantial 75 percent indicated the presence of anxiety symptoms. Within the anxiety group, a notable percentage, around 17 percent, fell into the moderate category of severity, and approximately 13 percent reported experiencing severe anxiety.
To quantitatively assess the immune cell profiles, blood samples were systematically collected from each participant. These samples underwent rigorous laboratory analysis to enumerate and characterize different types of NK cells. The study focused on two principal subgroups of NK cells. The first, identified as CD16+CD56dim cells, represents the predominant subset found within the peripheral nervous system, which serves as the crucial communication link between the central nervous system and the rest of the body. This particular subtype is characterized by its potent cytotoxic capabilities, meaning it possesses the inherent ability to directly identify and destroy cells that pose a threat to the organism, such as virus-infected cells or tumor cells. The second identified subgroup, known as CD16+CD56high cells, is comparatively less abundant. These cells play a vital role in orchestrating immune responses through the release of signaling molecules, or cytokines, which act as chemical messengers to modulate immune activity and promote immunoregulation. Both of these identified subgroups are classified as circulating NK cells, meaning they are found in the bloodstream.
The investigation meticulously examined how reported levels of anxiety and insomnia correlated with specific changes in NK cell populations. The results unequivocally demonstrated that students who reported experiencing anxiety symptoms exhibited a statistically significant reduction in both the relative proportion and the absolute count of circulating NK cells, encompassing both of their major subtypes, when compared to students who reported no anxiety symptoms. Furthermore, the study revealed a dose-dependent relationship between the severity of anxiety and the observed immune changes. Specifically, students reporting moderate to severe anxiety symptoms displayed a markedly reduced percentage of circulating NK cells. In contrast, those with only minimal or mild anxiety symptoms showed a decrease in NK cell percentages that was both small and not statistically significant, underscoring the impact of higher anxiety levels. Intriguingly, among students experiencing insomnia symptoms, a higher reported score for anxiety was directly associated with a diminished proportion of total peripheral NK cells, suggesting a synergistic effect of these two conditions on immune cell levels.
The implications of a decline in NK cell numbers and function are far-reaching, potentially weakening the body’s overall immune resilience. Such a compromised immune state can elevate the risk of developing a spectrum of health challenges. These can range from increased susceptibility to infectious diseases, due to a diminished capacity to clear pathogens, to a higher incidence of certain cancers, as the immune system’s surveillance mechanisms against abnormal cell growth are impaired. Moreover, chronic immune dysregulation associated with psychological distress can also contribute to the development or exacerbation of mental health conditions, such as depression, creating a complex feedback loop between mind and body. Dr. Alhamawi emphasized the clinical significance of these findings, stating, "Our understanding of how these psychological stressors influence the distribution and activity of immune cells, particularly peripheral NK cells, holds the potential to offer invaluable insights into the underlying biological mechanisms that contribute to chronic inflammation and the initiation and progression of tumors."
The researchers themselves acknowledged certain limitations inherent in their study design, which temper the broad applicability of their findings. A primary constraint was the exclusive inclusion of young female participants. This demographic group has, in recent years, experienced a disproportionate increase in the prevalence of both anxiety and sleep-related disorders, making them a particularly relevant but also specific population to study. Consequently, the observed associations may not be directly generalizable to other age groups, different sexes, or diverse geographical regions. The research team strongly advocated for the necessity of conducting further studies that encompass a wider spectrum of ages, both male and female participants, and a broader array of geographical locations. Such comprehensive research efforts are deemed essential for developing a more complete and nuanced understanding of how anxiety and insomnia exert their influence on NK cell levels and their functional capabilities across the general population.
The field of immunology and health psychology has long suggested that proactive lifestyle choices can play a significant role in bolstering immune function. Previous research has consistently indicated that adopting healthy habits, such as engaging in regular physical activity, effectively managing stress levels, and maintaining a balanced and nutrient-rich diet, can contribute to improved NK cell counts and enhanced immune system performance. Despite these established correlations, the pervasive nature of anxiety and insomnia can disrupt fundamental biological processes throughout the body, including the intricate mechanisms of immune response. This disruption, in turn, can act as a significant contributing factor to the development and persistence of chronic inflammatory diseases, which are implicated in a wide array of debilitating health conditions. In conclusion, Dr. Alhamawi summarized the overarching impact, stating, "Such detrimental impacts ultimately compromise an individual’s overall health and significantly diminish their quality of life."






