A groundbreaking clinical investigation is underway, offering a beacon of hope for individuals grappling with advanced dry age-related macular degeneration (AMD), a leading cause of irreversible vision impairment in older adults. This pervasive condition systematically erodes central vision, a crucial faculty for recognizing faces, deciphering text, and perceiving objects directly in one’s line of sight, often manifesting as progressively blurred areas, shadowy patches, or complete blind spots within the visual field. Currently, treatment avenues for this debilitating ailment, particularly its dry form, are exceptionally limited, underscoring the urgency for innovative therapeutic strategies.
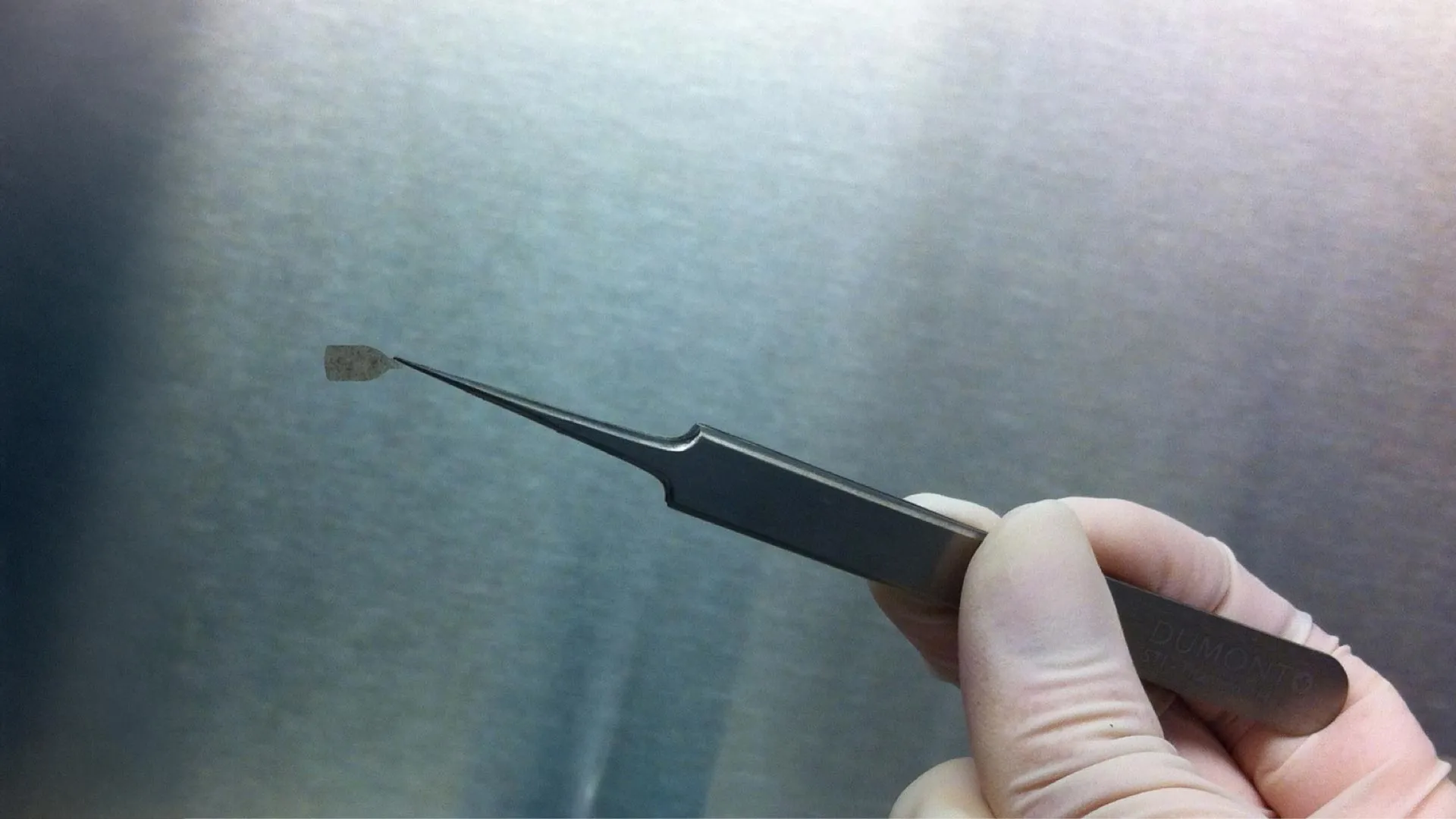
At the forefront of this pioneering research is the USC Roski Eye Institute, affiliated with Keck Medicine of USC, which has initiated a Phase 2b clinical trial designed to rigorously evaluate the efficacy of stem cell-based implants in rehabilitating compromised retinal cells and potentially re-establishing lost sight. The core of this experimental therapy involves an exquisitely engineered, ultra-thin implant, significantly more delicate than a human hair, meticulously crafted to securely anchor laboratory-grown stem cells within the eye. This sophisticated design aims to ensure the sustained viability and functional integration of these replacement cells into the existing retinal architecture.
Dr. Sun Young Lee, a distinguished retinal surgeon at Keck Medicine and the principal investigator overseeing the Keck Medicine study site, articulated the trial’s ambitious objectives. "Our primary aim is to ascertain whether this stem-cell derived retinal implant can not only halt the relentless progression of dry age-related macular degeneration but, more profoundly, stimulate a tangible improvement in patients’ visual acuity," Dr. Lee explained. She further emphasized the potentially transformative nature of these findings, noting, "While existing treatments can indeed slow the disease’s advance, none possess the capacity to reverse the damage already inflicted. This study represents a pivotal step toward that long-sought goal."
This contemporary trial builds upon a foundation of promising preliminary research conducted by specialists at the USC Roski Eye Institute. An initial, smaller-scale study yielded encouraging data, demonstrating the implant’s inherent safety profile, its secure and stable positioning within the ocular environment, and its successful assimilation into the retinal tissue. Crucially, a notable percentage of participants in that early phase reported experiencing some degree of vision enhancement, a finding that paved the way for the current, more extensive investigation. Dr. Lee elaborated on the significance of these prior results: "The initial phase of the clinical trial unequivocally established the treatment’s safety and its potential to positively impact patients’ vision; this subsequent phase is dedicated to rigorously assessing whether the therapy can achieve clinically meaningful visual improvements."
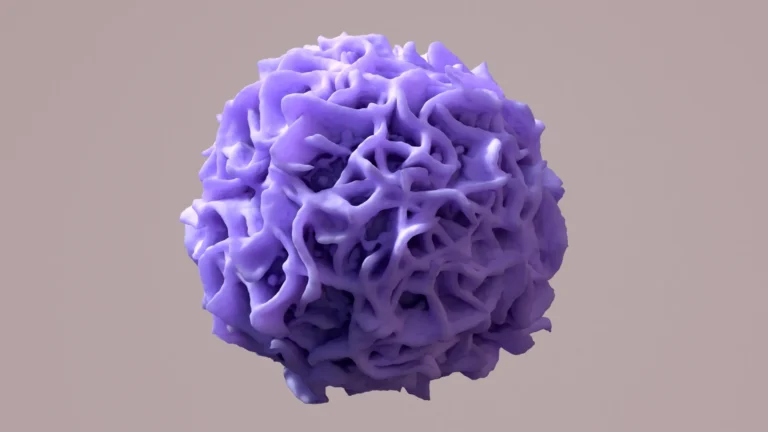
The intricate mechanism of the retinal implant is designed to address the fundamental pathology of AMD. Approximately 20 million Americans are affected by age-related macular degeneration, a demographic that encompasses both the dry and less common but often more severe wet forms of the disease. AMD primarily targets the macula, a minuscule yet vital region at the retina’s center responsible for sharp, detailed, and color vision. In the advanced stages of the disease, specialized cells known as retinal pigment epithelium (RPE) cells undergo damage or cease to function, a critical failure that directly precipitates visual decline. These RPE cells are indispensable for nourishing and supporting the photoreceptor cells responsible for detecting light.
The bioengineered implant at the heart of this clinical trial is meticulously fabricated from embryonic stem cells. These cells are cultured and differentiated in a controlled laboratory setting until they mature into functional RPE cells. During a minimally invasive outpatient surgical procedure, expert eye surgeons at Keck Medicine will precisely implant a delicate sheet of these lab-generated RPE cells directly onto the retina, aiming to replace the compromised or lost native cells. Dr. Rodrigo Antonio Brant Fernandes, an ophthalmologist at Keck Medicine and the study surgeon, detailed the implant’s intended function: "This study seeks to determine if the lab-engineered implant can effectively assume the roles of the damaged cells, perform as healthy RPE cells would, and ultimately enhance the vision of patients who currently have very few, if any, alternative options for improvement."
Keck Medicine is among a select group of five medical centers nationwide participating in this critical clinical trial. The study employs a masked design, meaning that a portion of the enrolled participants will receive the active bioengineered implant, while others will undergo a sham procedure designed to mimic the surgical process without the implantation of the therapeutic cells. This methodology is essential for isolating the true effects of the implant and mitigating potential placebo effects.
Eligibility criteria for participation are stringent, designed to identify individuals most likely to benefit from this experimental treatment. Candidates must fall within the age range of 55 to 90 years and have been diagnosed with advanced dry age-related macular degeneration characterized by geographic atrophy. Geographic atrophy signifies a progressive degeneration of the RPE cells and the overlying photoreceptors, leading to distinct blind spots.
Participants will be closely monitored for a minimum of one year, allowing researchers to meticulously assess the implant’s tolerability, track any adverse events, and document any observed changes in visual function. The trial is slated to enroll a total of 24 patients. Individuals interested in learning more about this groundbreaking trial or inquiring about potential participation are encouraged to contact Mariana Edwards at [email protected] or Kimberly Rodriguez at [email protected].
The USC Roski Eye Institute is deeply committed to advancing innovative therapeutic approaches that aim to restore vision and significantly enhance the quality of life for individuals affected by retinal diseases. Dr. Mark S. Humayun, co-director of the USC Roski Eye Institute, director of the USC Ginsberg Institute for Biomedical Therapeutics, and the Dennis and Michele Slivinski Chair in Macular Degeneration Research at the Keck School of Medicine, expressed his optimism for the future of stem cell-based therapies. "Stem cell-derived retinal implants hold immense promise as a transformative treatment for patients suffering from dry age-related macular degeneration, and we envision a future where such technologies could potentially offer a cure for this devastating condition," Dr. Humayun stated.
The sophisticated bioengineered RPE retinal implant utilized in this clinical trial is a product of Regenerative Patch Technologies LLC, a company dedicated to developing cutting-edge stem cell-based implants for a range of retinal disorders. Dr. Humayun is a co-inventor of this implant and a co-founder of the company, underscoring his deep involvement in its development from conception to clinical application. The proprietary technology underpinning the implant’s manufacture is exclusively licensed to Regenerative Patch Technologies by a consortium of leading academic institutions: the University of Southern California, the California Institute of Technology, and the University of California Santa Barbara. Financial support for this crucial clinical trial is generously provided, in part, by the California Institute for Regenerative Medicine, the Marcus Foundation, and USC, collectively enabling the advancement of this vital research.