This inherent difficulty in optimizing depression management stems largely from a deficiency in concrete, objective diagnostic instruments capable of forecasting an individual’s likely response to specific interventions. The prevailing paradigm for treatment selection relies predominantly on symptom profiles, patient histories, and clinician experience, rather than on definitive biological indicators. In an endeavor to explore novel avenues for MDD treatment and to ascertain the potential of neuroimaging in predicting therapeutic efficacy, a recent scientific investigation, detailed in the esteemed journal General Psychiatry, embarked on an ambitious exploration.
The cornerstone of this research was a rigorously designed randomized, double-blind, placebo-controlled clinical trial, meticulously conducted with 28 outpatients diagnosed with MDD at the Fourth People’s Hospital of Taizhou. The randomized nature of the trial ensured that participants were allocated to distinct treatment arms through impartial chance, thereby minimizing systematic bias. The double-blind protocol, wherein neither the participants nor the research personnel were privy to the specific treatments administered, further enhanced the objectivity of the findings. Complementing these measures, the placebo-controlled framework enabled a direct comparison of the effects of active interventions against the impact of inert substances.
Participants were systematically segregated into two distinct cohorts. The first cohort was administered Yueju Pill, a meticulously formulated traditional Chinese herbal medicine, in conjunction with a placebo designed to mimic escitalopram. Conversely, the second cohort received escitalopram, a widely recognized and commonly prescribed antidepressant medication, accompanied by a placebo engineered to resemble Yueju Pill. This sophisticated experimental design facilitated a direct and controlled comparison between the two therapeutic modalities under virtually identical conditions.
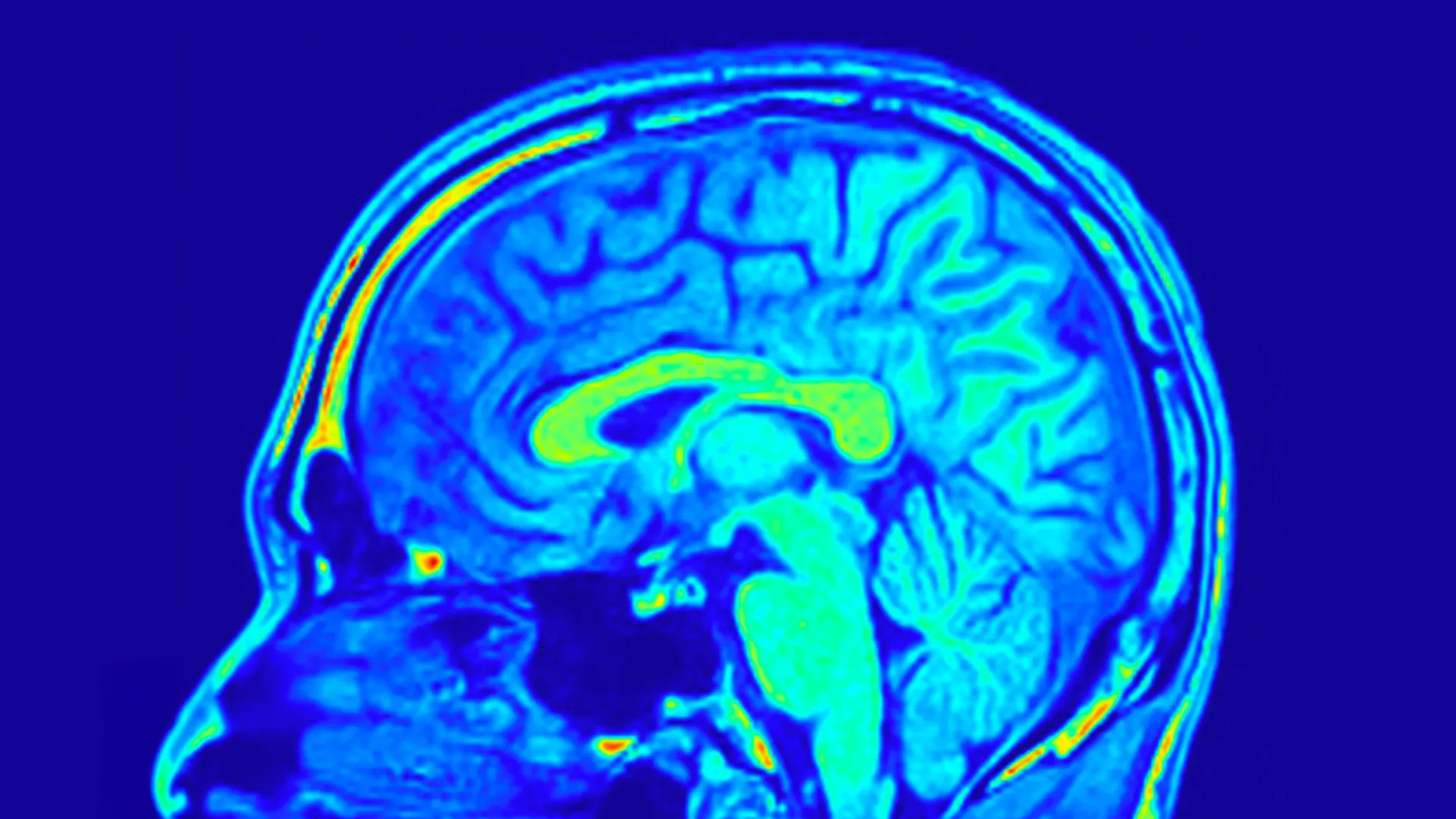
To comprehensively assess treatment outcomes, the research team employed the widely validated 24-item Hamilton Depression Scale (HAMD-24), a standardized clinical questionnaire, to quantify the severity of depressive symptoms. In parallel, biological data was meticulously collected, including peripheral blood samples and magnetic resonance imaging (MRI) brain scans, with the explicit aim of discerning alterations in brain structure and underlying biological processes.
Upon conclusion of the treatment period, a comparative analysis revealed that both therapeutic regimens elicited notable improvements in depressive symptomatology, suggesting a comparable efficacy between Yueju Pill and escitalopram in mitigating the overt clinical manifestations of depression. However, a crucial divergence emerged at the biological level. Specifically, it was observed that only participants who received Yueju Pill exhibited a statistically significant elevation in serum brain-derived neurotrophic factor (BDNF). BDNF, a vital protein instrumental in fostering neuronal growth, enhancing neural connectivity, and regulating mood, has been consistently associated with depression when found at diminished levels. This finding, therefore, carries considerable scientific weight.
The neuroimaging data provided even more profound and nuanced insights into the differential effects of the treatments. The researchers identified that distinct neural networks, comprising interconnected brain structures, possessed the capacity to prognosticate changes in depression scores within both treatment groups. These networks serve as a functional representation of how different brain regions are organized and communicate with each other.
Of particular significance was the observation that certain brain patterns demonstrated predictive power exclusively in individuals undergoing treatment with Yueju Pill. These predictive patterns were derived from measurements of sulcus depth and cortical thickness, parameters that delineate the intricate folding of the brain’s surface and the depth of its outermost layer, respectively. Both of these anatomical features are intrinsically linked to neurodevelopment and functional integrity. Further granular analysis indicated that the brain’s visual processing network played a particularly pivotal role in forecasting improvements in both depressive symptoms and BDNF levels among those administered Yueju Pill.
These converging findings strongly suggest that the identification of specific brain network configurations through MRI scans could serve as a powerful predictive biomarker for assessing individual patient responses to Yueju Pill therapy in the context of MDD. This innovative approach transcends the limitations of symptom-based diagnostic strategies, ushering in an era of more personalized and targeted antidepressant interventions.
Should these promising results be further substantiated through larger-scale clinical investigations, this neuroimaging-guided strategy could revolutionize clinical practice. It would empower clinicians to more precisely align patients with therapeutic interventions that possess a higher probability of success, thereby substantially reducing treatment delays and significantly improving patient outcomes. As articulated by Dr. Zhang, the lead author of the study, "The brain networks can then be fed to the predictive models constructed in this study to predict patients’ responses to Yueju Pill treatment. Based on the predicted responses, we can then determine whether the patient is suitable for Yueju Pill treatment." This research elegantly illustrates the potential of integrating established traditional medicinal practices with cutting-edge neuroimaging technologies to forge novel pathways toward precision medicine for depression.






