An estimated 65 million individuals globally are grappling with the protracted aftermath of SARS-CoV-2 infection, a condition now widely recognized as Long COVID, characterized by persistent symptoms extending beyond two months without an alternative medical explanation. Despite the substantial global burden, the medical community currently lacks approved, evidence-based therapeutic interventions specifically targeting this complex syndrome. Scientists worldwide are actively engaged in deciphering the intricate biological underpinnings of Long COVID, simultaneously exploring a broad spectrum of potential treatments ranging from structured rehabilitation protocols to novel pharmacological agents, including antivirals, anticoagulants, anti-inflammatory medications, nutritional supplements, and cutting-edge biologic therapies.
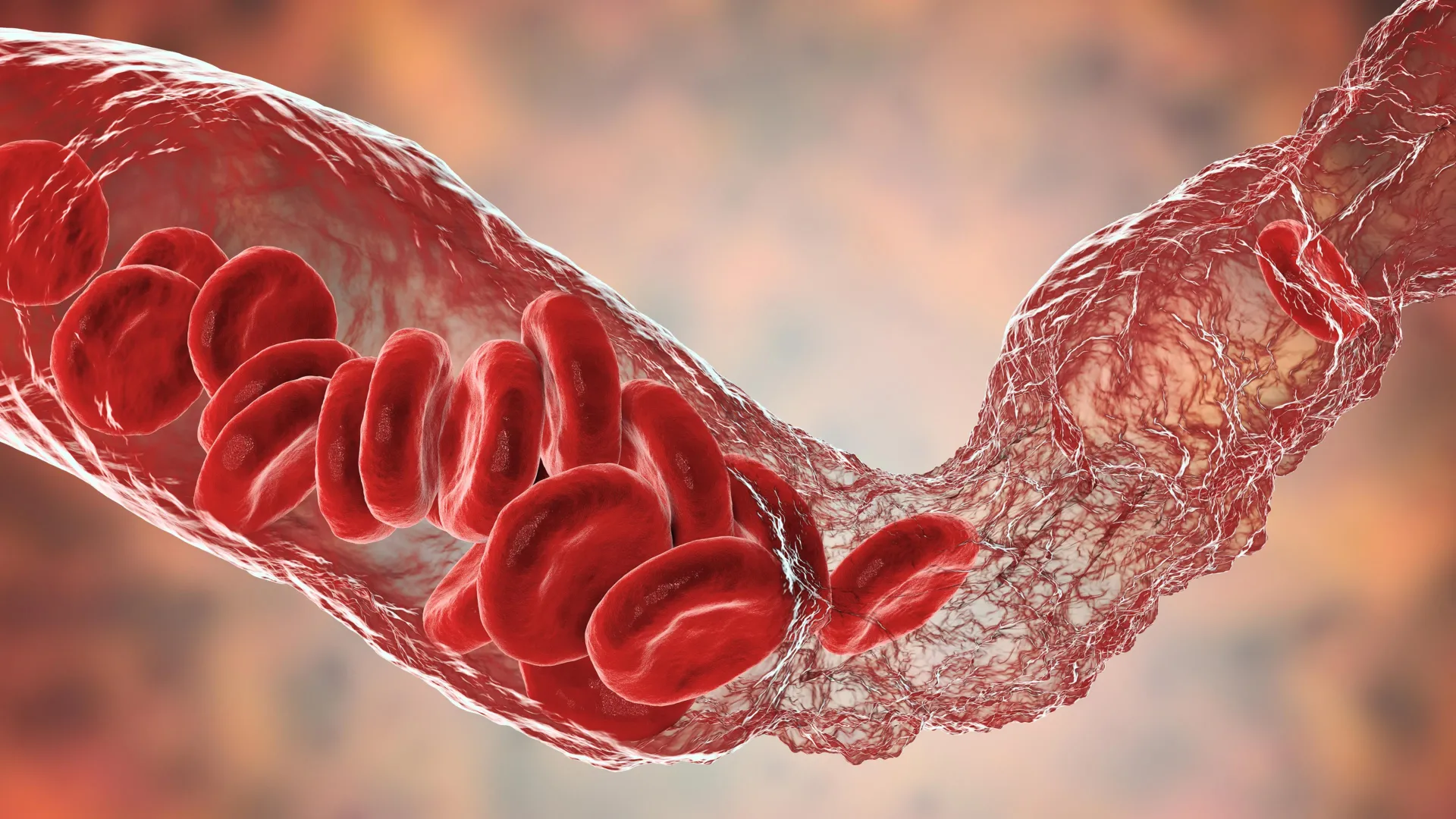
The prevailing scientific consensus suggests that Long COVID arises from a confluence of interconnected physiological disruptions. Among the most significant are the continued presence of viral remnants within the body, persistent low-grade systemic inflammation evidenced by elevated levels of cytokines such as Interleukin-1 beta (IL-1β), Interleukin-6 (IL-6), and Tumor Necrosis Factor-alpha (TNF-α), and the formation of minute blood clots. These microthrombi are believed to result from adverse interactions between the viral spike protein and fibrinogen, a key protein involved in blood clotting. Further contributing factors encompass the development of autoimmune responses, dysregulation of the gut microbiome, and impaired mitochondrial function, the cellular powerhouses responsible for energy production. The cumulative effect of these pathological processes can inflict damage across multiple organ systems, manifesting as compromised blood vessel function, cardiac inflammation, neuroinflammation, small fiber neuropathy, debilitating fatigue reminiscent of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), alterations in menstrual cycles, dysregulation of blood sugar homeostasis, and damage to the kidneys and liver.
For individuals experiencing milder symptoms in the initial phases of Long COVID, non-pharmacological interventions represent the primary line of defense. Clinical investigations have demonstrated that online, group-based physical and mental rehabilitation programs can significantly enhance patients’ quality of life. Furthermore, specific breathing exercises and inspiratory muscle training have shown efficacy in improving cardiopulmonary fitness. Additional supportive strategies may involve meticulous pacing of daily activities to prevent symptom exacerbation, cognitive and speech therapy to address neurological deficits, olfactory retraining to restore a sense of smell, and personalized dietary counseling. It is crucial to emphasize that physical activity programs must be implemented cautiously and progressively, with careful monitoring and adjustment based on individual symptom responses, as unsupervised or overly strenuous exercise can potentially amplify inflammation.
The administration of antiviral medications during the acute phase of COVID-19 infection appears to confer a modest protective effect against the subsequent development of Long COVID. In Japan, the antiviral ensitrelvir was associated with a 25% reduction in Long COVID incidence among outpatients. For individuals at higher risk of severe illness, nirmatrelvir/ritonavir and molnupiravir demonstrated an approximate 25% decrease in risk, while favipiravir exhibited limited benefit. Ongoing research is also investigating the potential of monoclonal antibodies designed to neutralize the viral spike protein, exploring their impact on neurotoxicity, though definitive results from Phase 3 trials are still pending.
A subset of therapeutic strategies is specifically designed to address distinct complications associated with Long COVID, including clotting disorders, autonomic nervous system dysfunction, and immune system imbalances. Low-dose naltrexone has shown promise in alleviating fatigue and reducing platelet aggregation. Apheresis, a procedure that filters the blood to remove micro-clots and auto-antibodies, offers temporary relief but is characterized by high costs and short-lived benefits. Other medications are currently undergoing evaluation for symptomatic management. Beta-blockers are employed to manage postural orthostatic tachycardia syndrome (POTS), a common autonomic dysfunction. Additionally, famotidine, intravenous immunoglobulin, sodium-glucose cotransporter-2 (SGLT-2) inhibitors, and glucagon-like peptide-1 (GLP-1) agonists are being investigated for their potential to ameliorate neurological, immune-related, cardiac, and renal manifestations of Long COVID.
Mitigating inflammation at its source represents a highly active area of therapeutic research. The early introduction of metformin, within seven days of infection, was linked to a 41% reduction in Long COVID risk, likely through its modulation of the mTOR signaling pathway. Plant-derived supplements such as quercetin, curcumin, and piperine have demonstrated improvements in fatigue levels compared to placebo. Other experimental approaches include sulfur-thermal water inhalation and the administration of enzymatically liberated salmon oil, both of which have been shown to decrease C-reactive protein (CRP) levels and support the lung’s protective barrier function. Baricitinib and rapamycin, drugs targeting the JAK and mTOR pathways respectively, are now being assessed in multi-center trials aimed at interrupting STAT3-driven systemic inflammation.
Modulating the gut microbiome is another promising avenue for therapeutic intervention. The synbiotic formulation SIM01 led to an improvement in overall symptoms after six months of use. Small-scale randomized trials suggest that high-dose supplementation with vitamins C and D, coenzyme Q10, magnesium, and creatine-glucose blends can enhance cellular energy production and improve vascular function. Early-stage studies have also reported benefits from N-acetyl-cysteine and the amino acid blend AXA1125, both of which have been shown to improve mitochondrial respiration and reduce fatigue.
Cutting-edge biologic treatments are exploring the critical role of fibrin in driving neuroinflammation. A humanized antibody designed to block the inflammatory domain of fibrinogen has shown protective effects against neuronal loss in preclinical studies and is currently in Phase 1 clinical trials. Another experimental therapy, the DNA aptamer BC007, targets auto-antibodies against G-protein-coupled receptors and has demonstrated reversal of fatigue and improvement in capillary blood flow in a single patient, although larger trials are necessary to confirm these findings. Beyond pharmacological interventions, non-drug approaches are also showing potential. Hyperbaric oxygen therapy, administered over a six-month period in a randomized trial, resulted in improvements in cognition, sleep quality, and pain. Case series reporting on acupuncture treatments have indicated reductions in brain fog and joint pain.
Vaccination against SARS-CoV-2 offers a limited degree of protection against Long COVID following breakthrough infections, reducing the risk by approximately 15% to 41%. For individuals already experiencing Long COVID symptoms, the outcomes following a booster vaccination were mixed: about 17% reported improvement, 21% experienced worsening symptoms, and 62% observed no significant change.
The current scientific landscape acknowledges that while numerous potential treatments exhibit early promise, the majority of evidence originates from small-scale or open-label studies relying on indirect outcome measures. There is an urgent need for large, adaptive randomized controlled trials that employ standardized definitions for Long COVID and utilize biomarker-based patient stratification to identify distinct subgroups. Until more definitive answers emerge, the consensus among experts advocates for a flexible, multidisciplinary approach. This strategy encompasses early antiviral therapy, carefully calibrated exercise regimens, targeted anti-thrombotic and anti-inflammatory interventions, support for gut microbiome health, and personalized rehabilitation plans. This comprehensive strategy acknowledges the complex, multi-system nature of Long COVID while research efforts continue to pursue definitive, mechanism-driven cures.







