The relentless pursuit of effective cancer treatments has long focused on harnessing the body’s intrinsic defenses. Despite significant advancements in immunotherapy, particularly with checkpoint inhibitors, a substantial number of patients still do not experience lasting benefits, highlighting the persistent challenge of tumor immune evasion. In a groundbreaking development, researchers at the University of Southampton have unveiled an innovative strategy to fundamentally re-engineer how the immune system perceives and confronts malignant cells, offering a potent new avenue for therapy. Their work, detailed in the prestigious journal Nature Communications, introduces a novel class of antibodies meticulously designed to dramatically amplify the activation signals crucial for anti-cancer T cell responses.
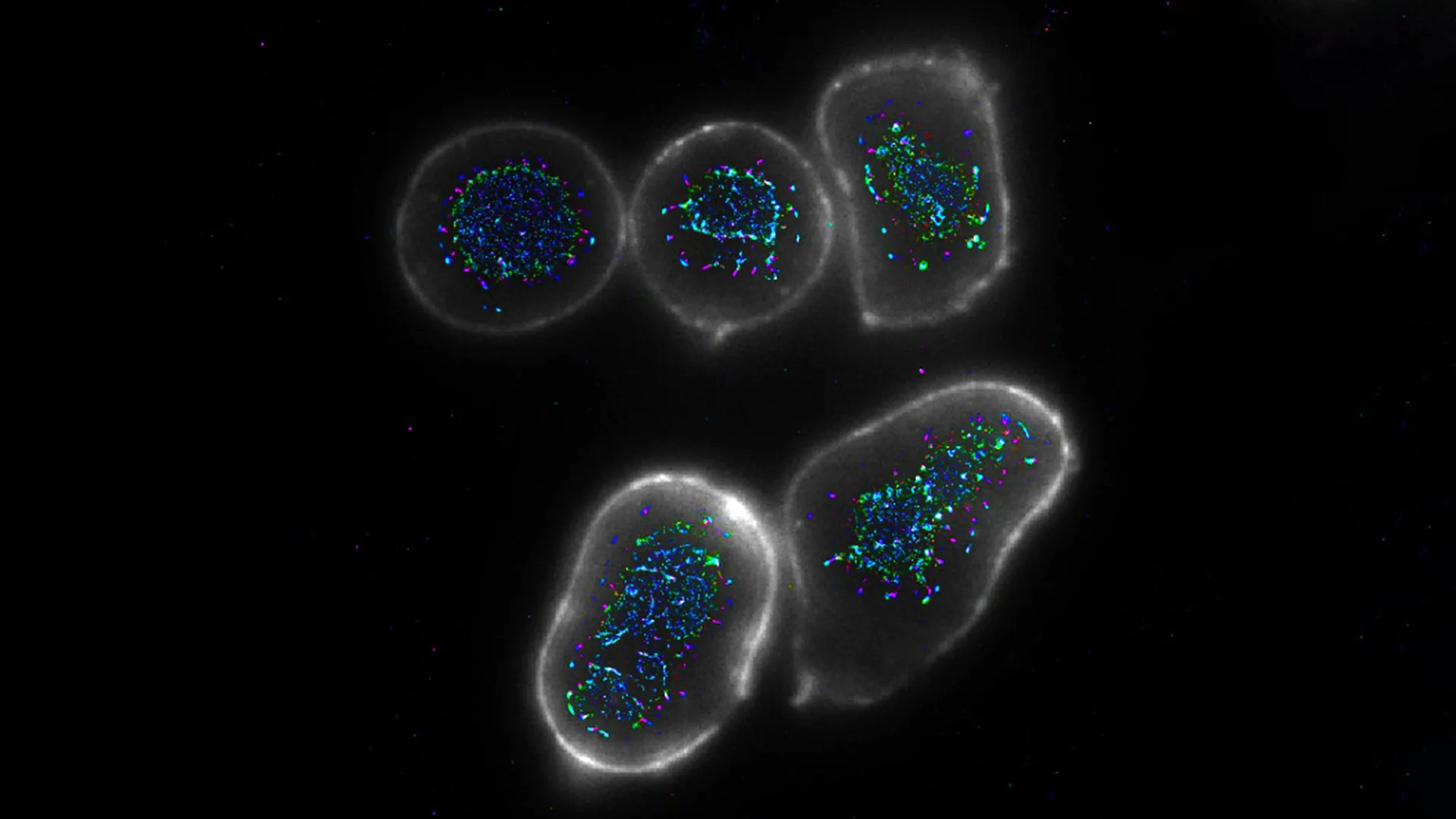
Understanding the intricate dance between the immune system and cancer is paramount to appreciating this breakthrough. At the forefront of the body’s anti-tumor arsenal are cytotoxic T lymphocytes, often referred to as CD8+ T cells. These highly specialized immune cells possess the remarkable ability to directly identify and eliminate cells that have become cancerous. They operate as vigilant sentinels, constantly patrolling the body for cellular anomalies. However, tumors are notoriously adept at developing sophisticated mechanisms to evade this immune surveillance. They can suppress T cell activity, create an immunosuppressive microenvironment, or simply fail to provide the necessary "go" signals that fully unleash a T cell’s cytotoxic potential.
Current immunotherapeutic approaches have revolutionized oncology by "unleashing the brakes" on T cells, effectively removing inhibitory signals that prevent them from attacking cancer. Drugs like PD-1/PD-L1 and CTLA-4 inhibitors have demonstrated remarkable success in various cancer types. Yet, their efficacy is not universal, and many patients either do not respond or eventually develop resistance. This underscores a critical need for complementary or alternative strategies that can directly "step on the gas," providing stronger, more decisive activation signals to T cells, especially in scenarios where natural activation is compromised.
The Southampton team’s research zeroes in on a specific co-stimulatory molecule known as CD27, expressed on the surface of T cells. CD27 plays a pivotal role in the optimal activation, proliferation, and survival of T lymphocytes. For a T cell to mount a robust and sustained attack against a pathogen or a cancer cell, it typically requires not just a signal recognizing the target, but also a secondary, co-stimulatory signal. CD27, when engaged by its cognate ligand, CD70, provides precisely such a crucial "boost." During healthy immune responses, cells infected with viruses or presenting antigens will naturally express CD70, thereby ensuring T cells receive a strong activation cue. The challenge in the context of cancer is that malignant cells frequently lack the expression of CD70. Without this essential ligand, T cells receive only a suboptimal or weak activation signal, leaving them functionally impaired and unable to effectively clear the tumor. This deficiency in CD70 expression by cancer cells represents a significant hurdle in harnessing the full power of the immune system for anti-cancer therapy.
Recognizing this critical gap, Professor Aymen Al Shamkhani, the principal investigator leading this pioneering work at the University of Southampton’s Centre for Cancer Immunology, and his team embarked on designing an entirely new class of therapeutic antibodies. Traditional therapeutic antibodies, while highly effective in various medical applications, typically adopt a Y-shaped structure with two binding arms (bivalent). This configuration limits their ability to simultaneously engage multiple receptor molecules on a cell surface, which is often crucial for generating a potent biological signal. For a receptor like CD27, which relies on spatial aggregation to transmit a strong activation signal, standard bivalent antibodies often fall short in mimicking the physiological clustering induced by its natural ligand.
The ingenuity of the Southampton team’s approach lies in their innovative antibody architecture. Instead of the conventional bivalent design, they engineered antibodies with four binding arms, rendering them tetravalent. This architectural enhancement allows for a significantly increased capacity to engage and bind to multiple CD27 receptors simultaneously on the surface of a T cell. However, mere binding is insufficient; the key to robust T cell activation lies in receptor clustering. To achieve this critical aggregation, these novel antibodies were designed with an additional strategic feature: they actively recruit a second type of immune cell, specifically those bearing Fc receptors. When these auxiliary cells bind to the constant region (Fc domain) of the engineered antibodies, they effectively pull together the antibodies, and consequently, the CD27 receptors bound by those antibodies. This induced spatial aggregation or "cross-linking" of CD27 receptors on the T cell membrane dramatically amplifies the downstream signaling pathways, closely replicating the intense and sustained activation signals that occur during a natural, highly effective immune response.
"Our foundational understanding of how the body’s endogenous CD27-CD70 axis orchestrates potent T cell activation was clear," explained Professor Al Shamkhani. "However, translating that intricate biological knowledge into a therapeutically viable molecule presented a formidable challenge. Antibodies are inherently stable and possess exquisite target specificity, making them excellent drug candidates. Yet, the conventional bivalent antibody format proved insufficient for optimally recapitulating the complex spatial dynamics required for robust CD27 signaling. This necessitated a complete re-imagination of antibody design to create a more functionally effective version."
The empirical validation of these quadravalent antibodies proved highly encouraging. Extensive laboratory tests, employing both human immune cells cultivated in vitro and sophisticated murine models in vivo, unequivocally demonstrated their superior agonistic activity. Compared to standard bivalent antibodies, the novel engineered constructs were vastly more effective at inducing the activation of CD8+ T cells. This enhanced activation was not merely a quantitative increase in cell signaling but translated into a profound functional improvement: the CD8+ T cells exhibited augmented proliferation, secreted higher levels of crucial effector cytokines, and, most importantly, displayed a significantly stronger anti-tumor response, effectively eradicating cancer cells in preclinical settings. These results provide compelling evidence that the targeted clustering of CD27 receptors via this novel antibody design can indeed unlock and unleash the full cytotoxic potential of T lymphocytes against malignant growths.
The implications of this breakthrough are far-reaching. By providing a method to precisely and potently activate a key co-stimulatory pathway (CD27) that is often underutilized in the context of cancer, this research lays a foundational blueprint for developing a new generation of immunotherapeutic agents. This innovative strategy offers a potential solution for patients who currently do not benefit from existing immunotherapies or for those whose tumors have developed resistance. Furthermore, these engineered antibodies could be deployed as standalone treatments or, perhaps more powerfully, as synergistic components within combination therapies, potentially enhancing the efficacy of checkpoint inhibitors or other modalities. The ability to effectively "turn up the volume" on T cell activation, even in challenging tumor microenvironments, holds immense promise for broadening the spectrum of cancer types amenable to immunotherapy and improving patient outcomes across various solid tumors and hematological malignancies.
The journey from laboratory discovery to clinical application is a rigorous one, involving further preclinical optimization, comprehensive toxicology studies, and ultimately, multiple phases of human clinical trials. However, the compelling data generated by the Southampton team strongly suggest that these quadravalent CD27-targeting antibodies represent a significant leap forward. "This sophisticated approach has the potential to substantially elevate the effectiveness of future cancer treatments," Professor Al Shamkhani further elaborated, "by enabling the immune system to operate at a level much closer to its inherent maximum potential, thereby providing a more decisive and enduring assault against cancer." This pioneering research was made possible through the critical funding and support provided by Cancer Research UK, underscoring the vital role of philanthropic investment in fueling innovative scientific endeavors at institutions like the University of Southampton’s Centre for Cancer Immunology, which continues to be at the forefront of advancing novel approaches in cancer immunotherapy.






