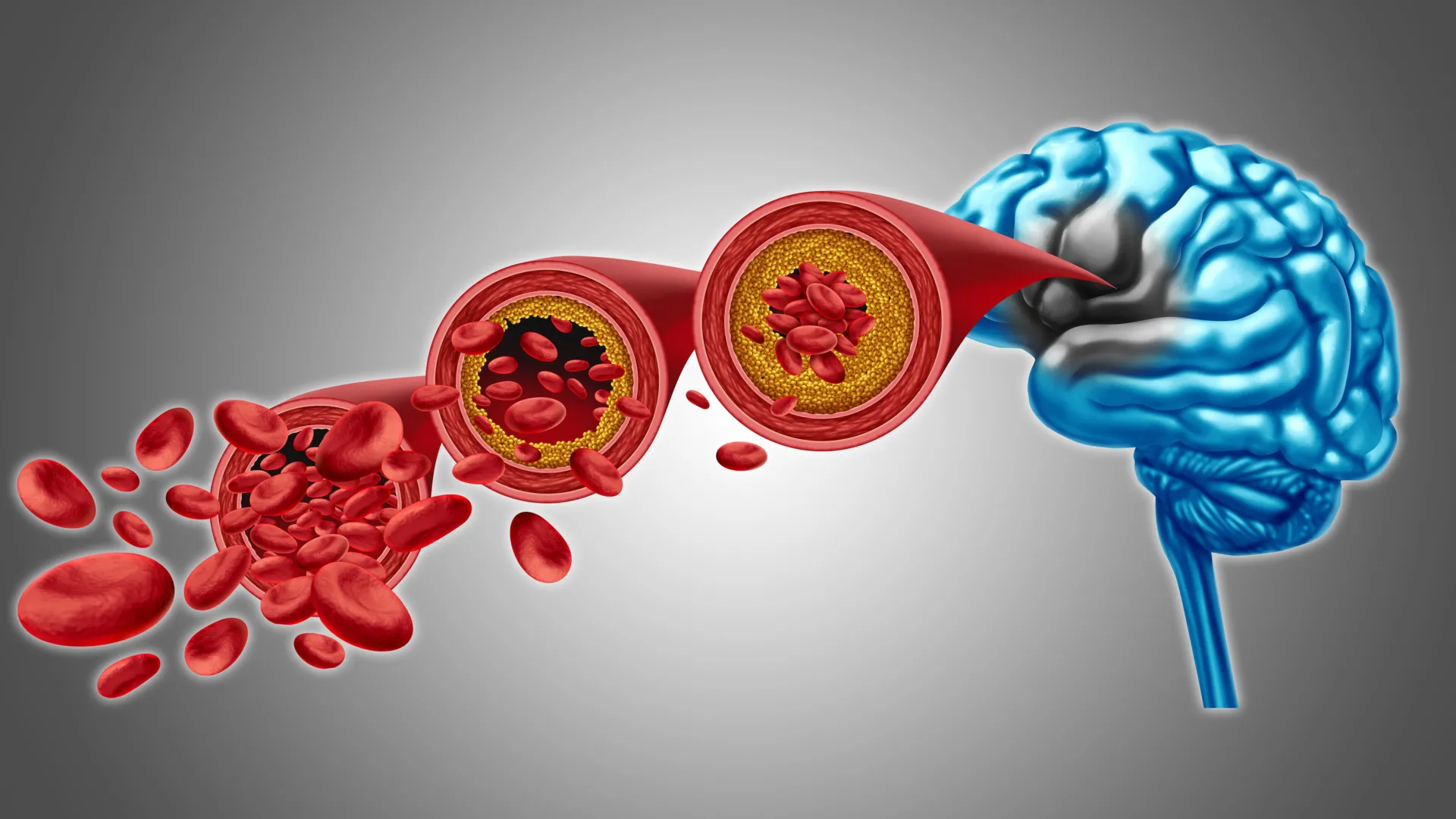
A groundbreaking scientific revelation from the University of Vermont’s Robert Larner, M.D. College of Medicine is illuminating a potential new avenue for combating reduced cerebral blood flow and specific forms of dementia. Researchers have meticulously detailed the intricate mechanisms governing brain circulation and have uncovered a promising method to potentially rectify vascular dysfunctions associated with these cognitive impairments. Their preclinical investigations, detailed in the December 22nd edition of the esteemed journal Proceedings of the National Academy of Sciences, propose that replenishing a deficient phospholipid within the bloodstream could be instrumental in re-establishing healthy brain blood flow and alleviating the debilitating symptoms characteristic of dementia.
"This discovery represents a significant leap forward in our pursuit of preventing dementia and neurovascular diseases," stated principal investigator Osama Harraz, Ph.D., an assistant professor of pharmacology at the Larner College of Medicine. "We are systematically unraveling the complex biological underpinnings of these profoundly challenging conditions, which now opens the door to conceptualizing the translation of this fundamental biological understanding into tangible therapeutic interventions."
The global impact of Alzheimer’s disease and other related dementias is substantial, affecting an estimated 50 million individuals worldwide, with projections indicating a continuous escalation of this figure. This escalating prevalence imposes an immense strain on individuals, families, professional caregivers, and the broader healthcare infrastructure. The scientific community is actively engaged in deciphering the multifaceted contributions of proteins, inflammatory processes, neural communication pathways, and cellular malfunctions to the pathogenesis of these neurological disorders.
The research conducted within Dr. Harraz’s laboratory specifically targets the regulation of cerebral blood flow and the intricate molecular signaling employed by blood vessels. A central element of their investigation revolves around Piezo1, a protein embedded within the cellular membranes of the endothelium, the inner lining of blood vessels. Piezo1 plays a crucial role in modulating brain blood flow by detecting the physical forces generated by the movement of blood through the brain’s complex vascular network. Its nomenclature is derived from the Greek word for "pressure," reflecting its mechanosensory function. Prior research had already indicated that Piezo1 exhibits altered behavior in individuals possessing specific genetic variations affecting the Piezo1 gene.
The recently published study, bearing the title "PIP2 Corrects an Endothelial Piezo1 Channelopathy," provides novel insights into the manner in which Piezo1 exerts its influence on cerebral blood flow. Critically, these findings also establish a link between conditions such as Alzheimer’s disease and the aberrant overactivity of Piezo1 within the blood vessels of the brain. To elucidate the reasons behind this phenomenon, the research team meticulously examined a phospholipid known as PIP2, a molecule naturally occurring within the membranes of brain cells.
PIP2 performs a vital function in cellular communication and the precise regulation of ion channels, a sophisticated process that governs the opening and closing of protein pores within cell membranes. The researchers made a pivotal discovery: PIP2 functions as a natural inhibitory agent of Piezo1. Consequently, when the levels of PIP2 diminish, Piezo1 becomes excessively active, leading to disruptions in the normal regulation of blood flow within the brain. In a critical experimental manipulation, the introduction of exogenous PIP2 into the system resulted in a reduction of Piezo1 activity and the restoration of healthy blood circulation. These compelling results strongly suggest that strategies aimed at augmenting PIP2 levels could serve as the foundation for an innovative therapeutic approach focused on enhancing brain blood flow and supporting optimal brain function.
Looking ahead, subsequent research endeavors will be dedicated to comprehensively understanding the precise molecular interactions between PIP2 and Piezo1. The scientific team aims to ascertain whether PIP2 binds directly to specific sites on the Piezo1 protein or whether it induces conformational changes in the surrounding cellular membrane that effectively restrict channel gating. Further investigations will also explore the mechanisms by which disease-induced reductions in PIP2 compromise this crucial regulatory control, thereby permitting Piezo1 to remain in a state of heightened activity and ultimately impairing cerebral blood flow. A thorough elucidation of these underlying mechanisms is paramount for the development of targeted therapies that aim to restore PIP2 levels or directly modulate Piezo1 activity to promote neurovascular health in the context of dementia and associated vascular pathologies.
The escalating global burden of neurodegenerative conditions like dementia underscores the urgent need for novel therapeutic strategies. These diseases, characterized by progressive cognitive decline, place immense emotional and financial strain on individuals and their support networks. The intricate interplay between vascular health and neuronal function has long been a subject of scientific inquiry, with evidence increasingly pointing towards compromised blood flow as a significant contributor to cognitive impairment. Understanding how the brain’s intricate vascular network maintains optimal perfusion is therefore central to developing effective interventions.
The discovery of Piezo1’s role in regulating cerebral blood flow marks a significant advancement in this field. As a mechanosensor, Piezo1 is uniquely positioned to translate the physical forces of blood flow into cellular signals that influence vascular tone and permeability. Its precise localization within the endothelial cells lining the cerebral vasculature suggests a direct role in fine-tuning blood delivery to specific brain regions. The observation that genetic variations in Piezo1 can influence its function in cerebrovascular regulation highlights the potential for personalized approaches to treatment.
The identification of PIP2 as a critical regulator of Piezo1 activity adds another layer of complexity and promise to this research. Phospholipids are fundamental components of cell membranes, involved in a vast array of cellular processes, including signal transduction, membrane trafficking, and protein function. PIP2, in particular, is known to interact with a multitude of cellular proteins, modulating their activity and localization. Its role as a natural suppressor of Piezo1 suggests a delicate balance that, when disrupted, can lead to pathological consequences.
The preclinical findings indicating that reduced PIP2 levels are associated with increased Piezo1 activity and subsequent impaired blood flow provide a compelling mechanistic link to dementia. This suggests that a deficit in this crucial phospholipid could be a direct driver of the vascular dysfunctions observed in these conditions. The experimental success in restoring normal blood flow by reintroducing PIP2 offers a tantalizing glimpse into a potential therapeutic intervention. This approach would aim to correct the underlying molecular imbalance, rather than solely addressing the downstream symptoms.
The future research directions outlined by the UVM team are crucial for translating these promising preclinical findings into clinical applications. A deeper understanding of the molecular interface between PIP2 and Piezo1 will be essential for designing targeted therapies. Whether PIP2 acts as a direct allosteric modulator, binding to a specific site on Piezo1 to alter its conformation, or indirectly influences Piezo1 activity by altering the biophysical properties of the cell membrane, will dictate the most effective therapeutic strategies. Moreover, pinpointing the specific disease-related pathways that lead to PIP2 depletion will be critical for identifying patient populations who might benefit most from such treatments.
The implications of this research extend beyond dementia. Neurovascular disorders encompass a broad spectrum of conditions, including stroke, vascular cognitive impairment, and even certain types of migraines, all of which involve disruptions in brain blood flow. Therefore, a therapeutic strategy that targets the fundamental mechanisms of cerebrovascular regulation could have far-reaching benefits. The challenge now lies in navigating the complex path from laboratory discovery to safe and effective clinical treatments, a journey that will require rigorous testing and validation.
The scientific community will be closely observing the progression of this research, hopeful that this novel understanding of the PIP2-Piezo1 axis will pave the way for much-needed therapeutic advancements in the fight against devastating neurological conditions. The potential to restore vital blood flow to the brain, thereby mitigating the ravages of dementia, represents a significant beacon of hope for millions worldwide.






