A groundbreaking clinical investigation is currently underway, offering a beacon of hope to millions worldwide grappling with the debilitating effects of age-related macular degeneration (AMD). This progressive ophthalmic condition stands as the foremost contributor to severe visual impairment and irreversible blindness among older adults in developed nations, particularly affecting individuals aged 65 and above. Researchers affiliated with the USC Roski Eye Institute, operating under the umbrella of Keck Medicine of USC, have initiated a pivotal Phase 2b clinical trial. This study aims to evaluate an innovative stem cell-based retinal implant designed to counteract the damage inflicted by advanced dry AMD, a form of the disease for which effective restorative interventions remain critically scarce.
The profound impact of AMD stems from its relentless assault on the macula, a minuscule yet indispensable region situated at the core of the retina. This specialized area is singularly responsible for facilitating sharp, detailed, and color vision, which is crucial for activities such as reading, facial recognition, and discerning objects directly within one’s gaze. As AMD progresses, individuals frequently encounter a deterioration of their central visual field, manifesting as blurred zones, obscured patches, or distinct blind spots that significantly impede daily functioning and diminish overall quality of life. The dry variant of AMD, which accounts for approximately 85-90% of all cases, is characterized by the gradual thinning of the macula and the accumulation of drusen, yellowish deposits beneath the retina. In its advanced stages, specifically geographic atrophy, crucial cells known as retinal pigment epithelium (RPE) cells undergo widespread degeneration or cease to function optimally. These RPE cells perform a vital supportive role for the photoreceptors—the light-sensing cells in the retina—by supplying nutrients and clearing waste products. Their demise directly precipitates the observed decline in visual acuity.
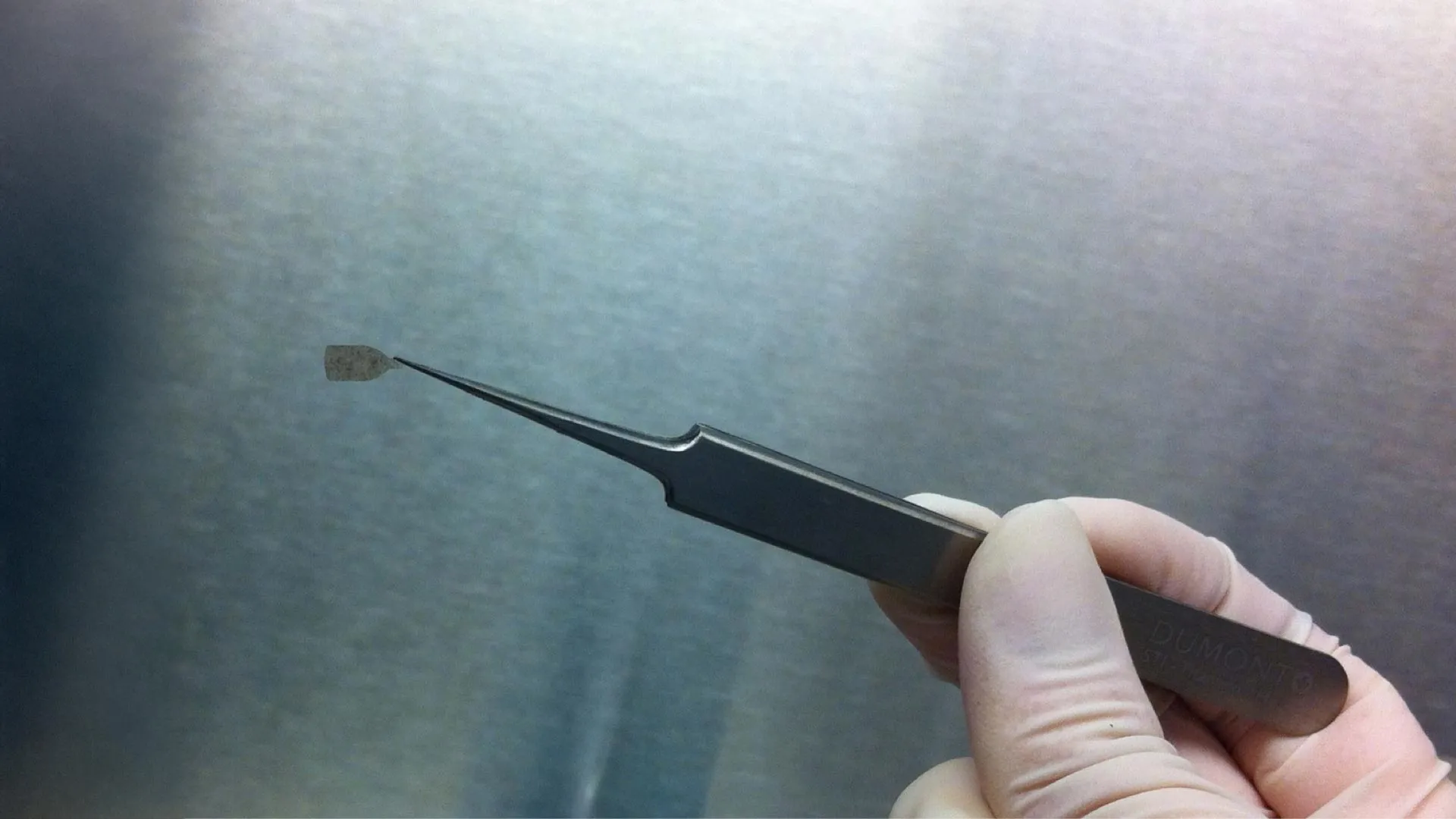
The investigational implant at the heart of this trial represents a sophisticated leap in regenerative medicine. It comprises RPE cells meticulously cultivated in a laboratory setting from embryonic stem cell lines. These pluripotent stem cells possess the remarkable capacity to differentiate into various specialized cell types, including the RPE cells required to replenish those lost in AMD. Once adequately matured, these lab-grown RPE cells are integrated onto an ultra-thin, biocompatible scaffold—an innovative design element that is finer than a human hair. This structural support is engineered to ensure the stable positioning and successful integration of the cells once surgically introduced into the ocular environment. The overarching hypothesis driving this therapeutic strategy is that by replacing the compromised RPE cells with healthy, functional ones, the progression of vision loss can be arrested, and, more ambitiously, some degree of visual function might be restored.
Dr. Sun Young Lee, a distinguished retinal surgeon at Keck Medicine and the principal investigator for the Keck Medicine arm of this multi-center study, articulated the ambitious goals of the trial. "Our objective extends beyond merely halting the insidious progression of dry age-related macular degeneration," Dr. Lee stated. "We are keenly focused on ascertaining whether this stem cell-based retinal implant possesses the capacity to genuinely enhance patients’ vision." She further emphasized the transformative potential of such findings, noting, "While contemporary ophthalmology offers a limited array of treatments primarily aimed at slowing the degenerative process of macular degeneration, there currently exists no therapeutic modality capable of reversing the visual damage that has already occurred. Success in this trial could redefine the treatment landscape for this prevalent condition." Dr. Lee also holds academic appointments as an associate professor of ophthalmology and physiology & neuroscience at the Keck School of Medicine of USC, underscoring her deep involvement in both clinical practice and scientific inquiry.
This current Phase 2b trial builds upon a foundation of promising outcomes from an earlier Phase 1/2a study. That preliminary investigation, conducted with a smaller cohort of patients, primarily focused on evaluating the safety profile of the implant and its surgical delivery method. The results from this initial phase were highly encouraging, demonstrating that the implant was well-tolerated by patients, maintained secure placement within the ocular cavity, and showed successful bio-integration into the existing retinal tissue. Crucially, the study observed that a notable proportion of participants—specifically 27%—experienced some measurable improvement in their visual capabilities. Dr. Lee reiterated the significance of these earlier findings, remarking, "The preceding phase of this clinical program provided robust evidence of the treatment’s safety and suggested a potential for beneficial effects on patient vision. This subsequent phase is designed to rigorously assess whether the therapy can achieve clinically meaningful and statistically significant enhancements in vision for a broader patient population."
The mechanism by which this bioengineered implant is intended to function is elegantly simple in concept, yet profoundly complex in execution. During an outpatient surgical procedure performed by experienced ophthalmic surgeons at Keck Medicine, the meticulously prepared thin layer of lab-grown RPE cells will be precisely positioned directly onto the patient’s retina. Dr. Rodrigo Antonio Brant Fernandes, an ophthalmologist with Keck Medicine and the lead study surgeon, elaborated on the therapeutic intent. "This study will meticulously investigate whether this laboratory-engineered implant can effectively assume the vital functions of the compromised RPE cells," Dr. Fernandes explained. "The ultimate aim is for these new cells to operate as healthy RPE cells would, thereby improving vision for individuals who currently face a dire prognosis with very few, if any, alternative pathways to visual restoration."
Approximately 20 million Americans are affected by some form of age-related macular degeneration, a figure that encompasses both the dry and wet forms of the disease. While the wet form is less common, accounting for about 10-15% of cases, it typically progresses more rapidly and can lead to more severe and sudden vision loss due to abnormal blood vessel growth beneath the macula. However, the sheer prevalence of the dry form, coupled with the absence of restorative therapies for its advanced stages, underscores the urgent clinical need that this stem cell trial seeks to address. The focus on patients with geographic atrophy is particularly pertinent, as this advanced manifestation of dry AMD is characterized by clearly demarcated areas of RPE cell death, making it an ideal target for cellular replacement strategies.
The current Phase 2b clinical trial is a multi-center endeavor, with Keck Medicine of USC serving as one of five select sites across the United States actively recruiting participants. To ensure the integrity and scientific rigor of the study, it employs a masked, or "blinded," design. This means that neither the participants nor the treating clinicians will know whether an individual patient is receiving the actual stem cell implant or undergoing a simulated surgical procedure, thereby minimizing potential bias in the evaluation of outcomes. Prospective patients seeking to qualify for the trial must meet specific eligibility criteria, including an age range of 55 to 90 years. Furthermore, they must have a confirmed diagnosis of advanced dry age-related macular degeneration alongside documented geographic atrophy, indicating a significant and irreversible loss of RPE cells.
Each enrolled participant will undergo a comprehensive follow-up period spanning at least one year. During this time, the research team will meticulously monitor various parameters, including the implant’s tolerance within the eye, the safety profile of the procedure, and, critically, any quantifiable changes in visual function. The study has a defined enrollment target of 24 patients in total, a number deemed sufficient for evaluating efficacy in this phase of clinical development. Individuals who meet the preliminary criteria and are interested in learning more about participation can contact the study coordinators, Mariana Edwards or Kimberly Rodriguez, via the provided institutional email addresses.
Looking beyond the immediate scope of this trial, leaders in ophthalmology envision a transformative future for stem cell-based ocular treatments. Dr. Mark S. Humayun, co-director of the USC Roski Eye Institute, director of the USC Ginsberg Institute for Biomedical Therapeutics, and the Dennis and Michele Slivinski Chair in Macular Degeneration Research at the Keck School, articulated this long-term vision. "The USC Roski Eye Institute remains steadfast in its commitment to pioneering innovative therapeutic modalities aimed at enhancing and restoring vision, thereby profoundly improving patients’ lives," Dr. Humayun asserted. "Stem cell-derived retinal implants, such as the one currently under investigation, represent one of the most promising avenues for patients afflicted with dry age-related macular degeneration. Indeed, they hold the potential to offer not just treatment, but perhaps, one day, a genuine cure for this devastating condition."
The development and production of this bioengineered RPE retinal implant are the result of collaborative efforts involving Regenerative Patch Technologies LLC, a clinical-stage biotechnology firm dedicated to advancing stem cell-based implants for a range of retinal diseases. Dr. Humayun’s integral role extends to being a co-inventor of this innovative implant and a co-founder of the company. The proprietary technology underpinning the manufacturing of this implant is exclusively licensed to Regenerative Patch Technologies through a tripartite agreement involving the University of Southern California, the California Institute of Technology, and the University of California Santa Barbara. Financial support for this crucial clinical trial has been generously provided by multiple entities, including significant contributions from the California Institute for Regenerative Medicine, the Marcus Foundation, and the University of Southern California itself, underscoring the broad commitment to bringing this potentially life-changing therapy to fruition.






