Major Depressive Disorder (MDD) represents a profound and pervasive global health challenge, significantly impairing an individual’s cognitive processes, emotional regulation, and overall functional capacity in daily life. This severe mental health condition is already recognized as a primary global contributor to health burden and lost productivity, with projections indicating it could become the most prevalent and economically burdensome illness worldwide by the close of this decade. Despite the availability of numerous pharmacological interventions designed to alleviate depressive symptoms, the process of identifying the most effective medication for a specific patient remains an arduous and often protracted endeavor. A disheartening reality is that nearly one-third of individuals diagnosed with MDD do not experience adequate improvement following their initial antidepressant prescription, frequently subjecting them to an extended period of sequential medication adjustments, often referred to as a "trial-and-error" approach, which can span many months.
A fundamental obstacle hindering more efficient and effective treatment selection lies in the conspicuous absence of objective, quantifiable tools capable of predicting an individual’s likely response to a particular therapeutic regimen. Presently, clinical decisions concerning antidepressant prescriptions are predominantly guided by a subjective evaluation of symptoms, a patient’s medical history, and the clinician’s experiential knowledge, rather than being informed by precise biological indicators. This empirical method often leads to delays in achieving remission, prolonged suffering for patients, and increased healthcare costs. Against this backdrop, a recent groundbreaking investigation, published in the esteemed journal General Psychiatry, embarked on an ambitious quest to ascertain whether traditional Chinese medicine (TCM) could offer novel therapeutic insights into MDD treatment, and, crucially, if advanced brain imaging techniques could serve as reliable predictors of treatment efficacy.
The research team meticulously designed and executed a randomized, double-blind, placebo-controlled clinical trial, widely regarded as the gold standard for evaluating medical interventions. This rigorous methodology is paramount for minimizing bias and establishing a robust cause-and-effect relationship between treatment and outcome. The study involved a cohort of 28 outpatients, all formally diagnosed with MDD, who were recruited from the Fourth People’s Hospital of Taizhou. In a randomized trial, participants are allocated to different treatment arms purely by chance, ensuring that groups are comparable at baseline and that any observed differences in outcomes can be attributed to the intervention rather than pre-existing disparities. The double-blind aspect signifies that neither the study participants nor the investigators responsible for administering treatments and collecting data were aware of which specific intervention any individual received. This dual masking is critical for mitigating the influence of expectation biases from both patients (placebo effect) and researchers. Furthermore, the inclusion of a placebo-controlled design enabled the scientists to rigorously compare the genuine therapeutic effects of the active treatments against inert substances, thereby isolating the true pharmacological impact.
Participants were systematically divided into two distinct groups. One cohort was administered Yueju Pill, a traditional Chinese herbal formulation with a long history of use for mood-related conditions, concurrently with a placebo equivalent to escitalopram, a widely prescribed conventional antidepressant. The second cohort, in contrast, received escitalopram alongside a placebo designed to mimic Yueju Pill. This ingenious cross-over placebo design permitted a direct and unbiased comparison of the two distinct therapeutic approaches under precisely matched experimental conditions, thereby allowing researchers to delineate their respective mechanisms and efficacies.
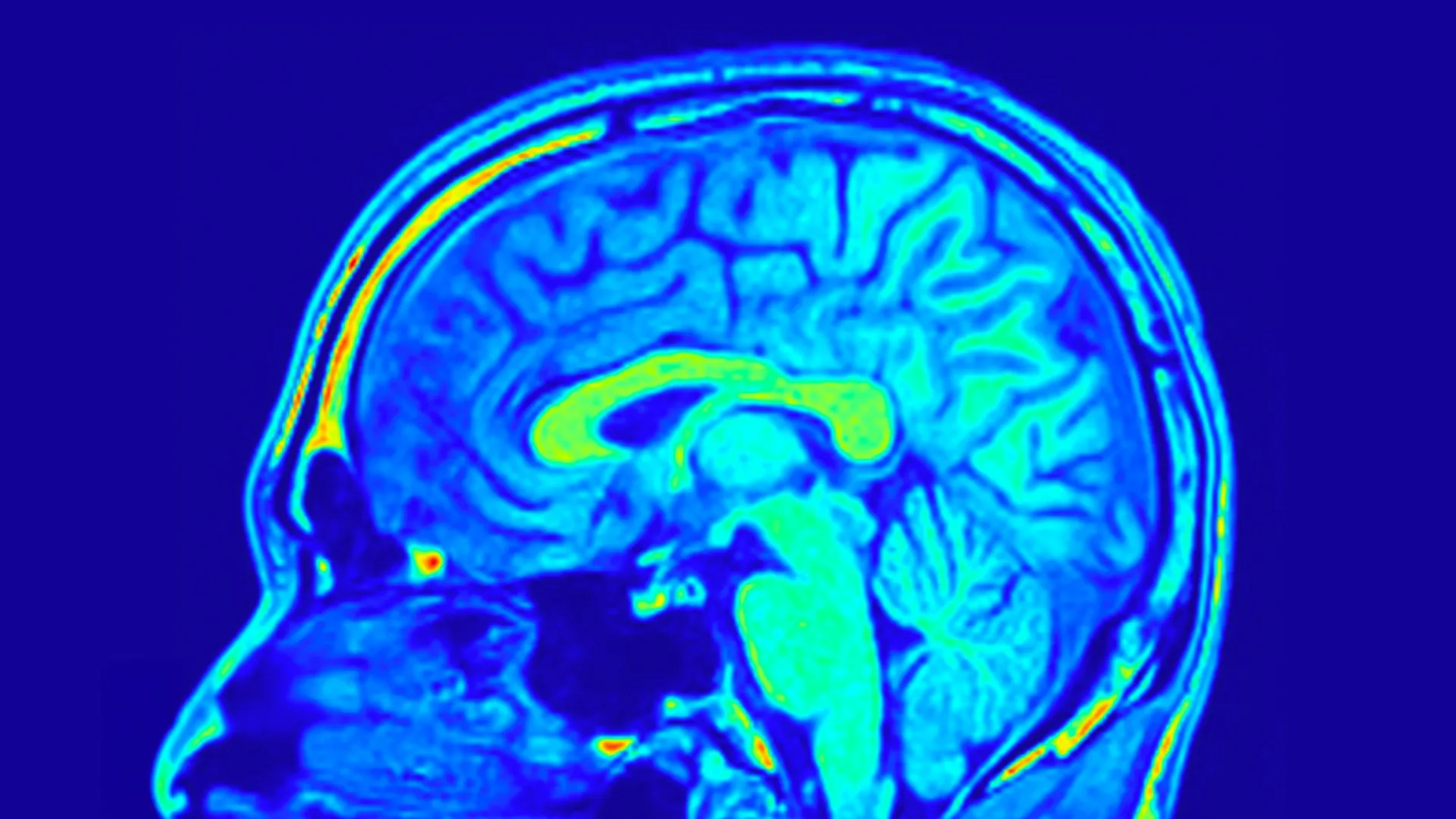
To meticulously monitor and quantify the therapeutic outcomes, the research team employed several sophisticated assessment tools. The primary measure of depression severity was the 24-item Hamilton Depression Scale (HAMD-24), a widely validated and extensively utilized clinical questionnaire that provides a standardized numerical score reflecting the severity of depressive symptoms. Beyond clinical symptom assessment, the study incorporated biological measurements: peripheral blood samples were collected from all participants to analyze various biochemical markers, and critically, magnetic resonance imaging (MRI) brain scans were performed. These advanced neuroimaging techniques were employed to scrutinize changes in both the structural architecture and the underlying biological processes within the brain, offering an objective window into the neural correlates of treatment response.
Following the prescribed course of treatment, a significant observation emerged: both participant groups exhibited measurable improvements in their depressive symptoms, as evidenced by reductions in their HAMD-24 scores. This finding suggested that both Yueju Pill and escitalopram demonstrated comparable effectiveness in mitigating the overt clinical manifestations of depression. However, a deeper dive into the biological data unveiled a crucial divergence in their mechanistic pathways. Specifically, only patients within the group receiving Yueju Pill experienced a statistically significant elevation in serum brain-derived neurotrophic factor (BDNF) levels. BDNF is a vital protein known for its multifaceted role in supporting neuronal growth, facilitating synaptic plasticity (the brain’s ability to adapt and form new connections), and modulating mood regulation. The consistent association of diminished BDNF levels with the pathophysiology of depression lends particular salience to this finding, indicating that Yueju Pill may exert its antidepressant effects, at least in part, through neurotrophic mechanisms.
The brain imaging data, however, provided an even more profound layer of insight into the neural underpinnings of treatment response. Researchers discovered that distinct networks, characterized by the intricate organization and connectivity patterns of various brain structures, possessed predictive power concerning the observed changes in depression scores across both treatment groups. These "networks" are essentially functional or structural alliances between different brain regions, reflecting how various parts of the brain communicate and coordinate their activities. The analysis demonstrated that the inherent organization of these neural circuits could offer clues about an individual’s propensity to respond to antidepressant therapy.
More remarkably, the study uncovered specific patterns within the brain’s architecture that were exclusively predictive for patients undergoing treatment with Yueju Pill. These unique predictive patterns were derived from analyses of sulcus depth and cortical thickness. Sulcus depth refers to the extent of the infoldings or grooves on the brain’s surface, while cortical thickness describes the thickness of the brain’s outermost layer, the cerebral cortex, which is crucial for higher cognitive functions. Both sulcus depth and cortical thickness are fundamental anatomical features closely associated with brain development, maturation, and overall neurological function. Further detailed analysis revealed that the brain’s visual network played an exceptionally salient role in predicting improvements in both depressive symptoms and the aforementioned BDNF levels among those individuals treated with the traditional Yueju Pill. This suggests a specific neural signature tied to the efficacy of this particular herbal remedy.
Collectively, these compelling findings strongly indicate that the identification of specific brain network patterns through advanced MRI scans holds immense promise for predicting how individual patients suffering from MDD might respond to treatment with Yueju Pill. This innovative approach represents a significant departure from the current symptom-based decision-making paradigm, pointing towards a future where antidepressant therapy can be precisely tailored to an individual’s unique neurobiological profile.
The implications of this research are far-reaching. If these findings are robustly validated in subsequent, larger-scale studies involving more diverse patient populations, this strategy could revolutionize clinical practice. It would empower clinicians to proactively match patients with the specific therapeutic interventions that are most likely to be effective for them from the outset. Such precision would dramatically reduce the agonizing delays associated with the current trial-and-error approach, mitigate patient suffering, minimize healthcare expenditures, and ultimately lead to significantly improved long-term outcomes for individuals battling depression. As Dr. Zhang, the principal author of the study, articulated, "The brain networks can then be fed to the predictive models constructed in this study to predict patients’ responses to Yueju Pill treatment. Based on the predicted responses, we can then determine whether the patient is suitable for Yueju Pill treatment." This vision outlines a future where a patient’s brain scan could guide their initial prescription, eliminating much of the current guesswork.
This pioneering investigation underscores the immense potential inherent in integrating established traditional medical practices with cutting-edge modern neuroimaging technologies. Such a convergence offers a potent pathway toward developing a truly personalized and precise approach to the management and treatment of major depressive disorder. It marks a significant step forward in the quest to move beyond symptomatic relief towards a more biologically informed and individualized psychiatric care model, offering renewed hope for millions affected by this debilitating condition. While further research is imperative to validate and expand upon these findings, the study lays a critical foundation for an era where psychiatric interventions are as precise and effective as those in other fields of medicine.






