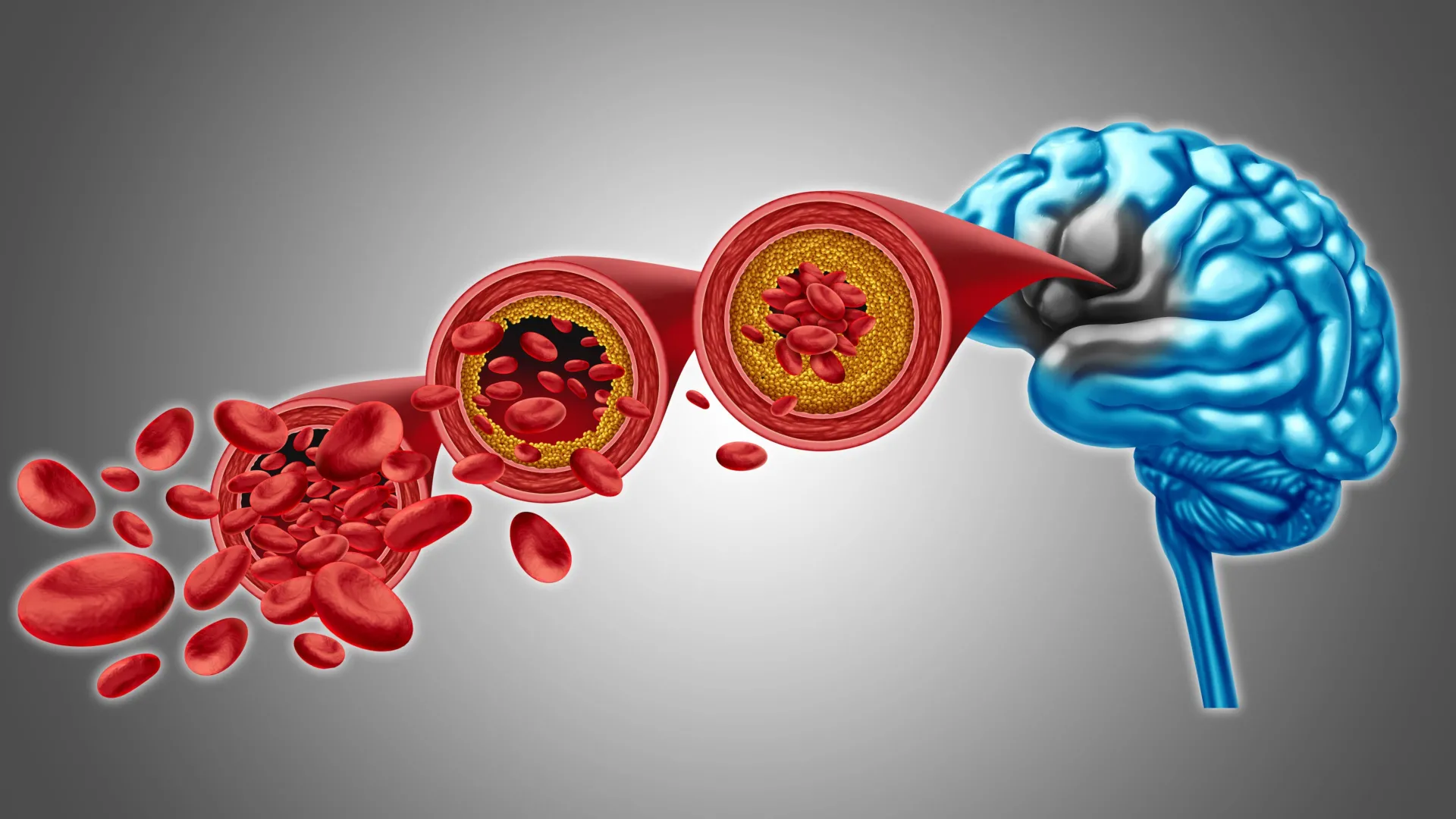
A significant stride toward potentially reversing compromised brain blood flow and mitigating certain forms of cognitive decline has been illuminated by researchers at the University of Vermont’s Robert Larner, M.D. College of Medicine. Their groundbreaking preclinical investigations, detailed in the December 22nd edition of the esteemed journal Proceedings of the National Academy of Sciences, have elucidated crucial details regarding the intricate mechanisms governing cerebral vasculature and the potential to rectify associated dysfunctions. The findings suggest that replenishing a specific, depleted phospholipid within the circulatory system could be instrumental in re-establishing healthy brain blood flow and alleviating symptoms characteristic of dementia.
"This breakthrough represents a monumental leap forward in our quest to combat dementia and neurovascular diseases," stated principal investigator Osama Harraz, Ph.D., an assistant professor of pharmacology at the Larner College of Medicine. "We are diligently unraveling the complex biological pathways underlying these debilitating conditions, paving the way for the eventual translation of this fundamental science into tangible therapeutic interventions."
The escalating global burden of dementia, encompassing conditions like Alzheimer’s disease, affects an estimated 50 million individuals worldwide, with projections indicating a continued upward trajectory. This growing prevalence exerts immense strain on familial support networks, professional caregivers, and the broader healthcare infrastructure. Current research endeavors are intensely focused on dissecting the multifaceted contributions of protein aggregation, inflammatory processes, neural signaling anomalies, and cellular dysfunction to the pathogenesis of these disorders.
Within the Harraz laboratory, a primary area of inquiry revolves around the precise regulation of cerebral blood flow and the intricate molecular dialogue orchestrated by blood vessels. A central element of this research is Piezo1, a mechanosensitive protein embedded within the membranes of endothelial cells lining the brain’s blood vessels. Piezo1 plays a pivotal role in modulating cerebral blood flow by detecting the physical forces generated by blood coursing through the brain’s vascular network. Its nomenclature is derived from the Greek word for "pressure," reflecting its fundamental function. Prior studies have indicated that the behavior of Piezo1 can vary significantly in individuals possessing specific genetic variations of the Piezo1 gene.
The recently published study, provocatively titled "PIP₂ Corrects an Endothelial Piezo1 Channelopathy," offers profound new insights into the ways in which Piezo1 influences cerebral blood flow dynamics. Crucially, the research illuminates a correlation between conditions such as Alzheimer’s disease and an aberrant hyperactivity of Piezo1 within the cerebral vasculature. To thoroughly investigate this phenomenon, the research team meticulously examined a vital phospholipid known as PIP₂, which is a ubiquitous component of neuronal and vascular cell membranes.
PIP₂ performs an indispensable role in cellular communication pathways and the sophisticated regulation of ion channels – a complex biological process that dictates the precise timing and duration of the opening and closing of protein pores within cell membranes. The researchers made a pivotal discovery: PIP₂ functions as an endogenous inhibitory molecule, acting as a natural brake on Piezo1 activity. Consequently, when levels of PIP₂ diminish, Piezo1 becomes excessively active, thereby disrupting the finely tuned regulation of blood flow within the brain. In a critical experimental manipulation, the introduction of exogenous PIP₂ into the biological system led to a marked reduction in Piezo1 activity and a subsequent restoration of healthy blood circulation. These compelling findings strongly suggest that strategies aimed at augmenting PIP₂ levels could serve as the bedrock for novel therapeutic approaches designed to enhance cerebral blood flow and bolster overall brain function.
Looking ahead, subsequent research phases will be dedicated to comprehensively delineating the precise molecular interactions between PIP₂ and Piezo1. Scientists aim to ascertain whether PIP₂ directly binds to specific functional domains of the Piezo1 protein or whether it exerts its regulatory influence by subtly altering the biophysical properties of the surrounding cellular membrane, thereby limiting channel activation. Further investigations will also probe the mechanisms by which disease-associated reductions in PIP₂ levels precipitate a loss of this critical regulatory control, leading to persistent Piezo1 overactivity and the consequent impairment of cerebral blood flow. A profound understanding of these underlying biological mechanisms will be paramount for the development of effective therapeutic interventions that either restore PIP₂ levels or directly modulate Piezo1 activity to promote neurovascular health in the context of dementia and related cerebrovascular disorders. The implications of this research extend beyond immediate therapeutic targets, offering a deeper appreciation of the delicate balance required for optimal brain function and highlighting the critical role of vascular health in cognitive well-being. This work provides a crucial foundation for future translational research, moving from fundamental discovery towards clinical application.






