Major depressive disorder (MDD), a pervasive and debilitating mental health ailment, significantly disrupts an individual’s capacity to think, feel, and navigate daily responsibilities. Currently recognized as a primary driver of global disability, projections indicate that MDD will ascend to become the most prevalent and economically burdensome illness worldwide by the year 2030. Despite the availability of numerous pharmacological interventions, the process of identifying the most efficacious treatment for a given patient remains a formidable challenge. It is a well-established fact that approximately one-third of individuals diagnosed with depression do not experience meaningful improvement after commencing their initial antidepressant regimen, frequently necessitating an arduous and protracted period of therapeutic experimentation.
This inherent difficulty in treatment selection stems, in large part, from a deficit in readily accessible, objective diagnostic tools capable of forecasting which therapeutic approach will yield the optimal outcome for an individual. Consequently, clinical decisions regarding depression management are predominantly informed by an assessment of presented symptoms, a patient’s comprehensive medical history, and the practitioner’s accumulated experience, rather than by definitive biological indicators. In an effort to address this critical gap, a recent scientific inquiry, documented in the pages of the journal General Psychiatry, embarked on an investigation to ascertain whether the principles and remedies of traditional Chinese medicine (TCM) could offer novel perspectives on managing MDD, and crucially, whether advanced brain imaging techniques could serve as a predictive instrument for treatment efficacy.
The investigative team designed and executed a rigorous randomized, double-blind, placebo-controlled clinical trial, enlisting the participation of 28 outpatients who had received a diagnosis of MDD from the Fourth People’s Hospital of Taizhou. The cornerstone of this experimental design was randomization, a process by which participants were allocated to distinct treatment arms purely by chance, thereby mitigating potential systematic biases. The double-blind nature of the study ensured that neither the participants nor the researchers administering the treatments were privy to the specific interventions being received, further safeguarding against observer and participant expectation effects. Complementing this, the placebo-controlled framework enabled a direct comparison of the effects of active treatments against those of inert substitutes, isolating the true therapeutic impact.
Participants were strategically assigned to one of two investigative cohorts. The first cohort was administered Yueju Pill, a meticulously formulated herbal remedy rooted in traditional Chinese medicinal practices, concurrently with a placebo designed to mimic the appearance and administration of escitalopram. The second cohort received escitalopram, a widely recognized and frequently prescribed selective serotonin reuptake inhibitor (SSRI) antidepressant, in conjunction with a placebo designed to mirror Yueju Pill. This carefully constructed comparative design facilitated a direct and equitable evaluation of the two distinct therapeutic modalities under rigorously controlled conditions.
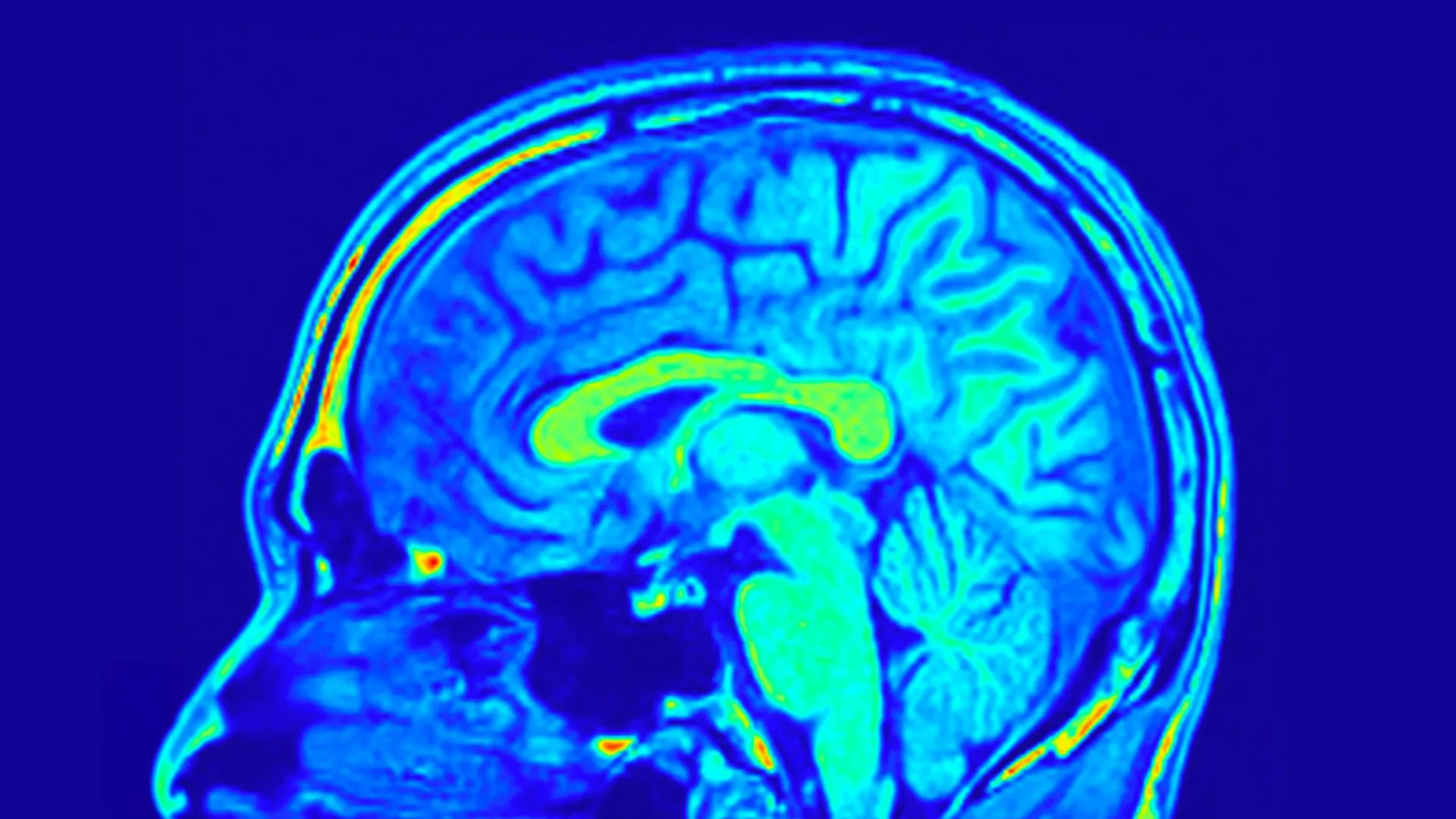
To comprehensively assess the impact of these interventions, the research team employed a multi-faceted approach to outcome measurement. The severity of depressive symptomatology was systematically quantified using the Hamilton Depression Rating Scale, specifically the 24-item version (HAMD-24), a psychometric instrument widely regarded as a gold standard in clinical depression assessment. In parallel, biological data were meticulously collected through the acquisition of peripheral blood samples, and advanced magnetic resonance imaging (MRI) scans of the brain were performed to meticulously examine alterations in both the structural architecture and the biochemical milieu of the brain.
Analysis of the post-treatment data revealed a compelling convergence of therapeutic efficacy. Both the Yueju Pill group and the escitalopram group exhibited statistically significant amelioration of their depression symptoms, indicating that both interventions were comparably effective in alleviating the overt clinical manifestations of the disorder. However, a critical divergence emerged at the molecular level. Notably, only the participants who received Yueju Pill demonstrated a significant augmentation in serum levels of brain-derived neurotrophic factor (BDNF). BDNF is a vital protein that plays a pivotal role in fostering neurogenesis, promoting synaptic plasticity, and critically, in the regulation of mood. The observed correlation between lower BDNF levels and the presence of depression in prior research renders this specific finding particularly significant, suggesting a potential mechanistic pathway for Yueju Pill’s antidepressant effects.
The insights gleaned from the brain imaging data offered an even more profound understanding of the underlying neurobiological changes. The researchers identified specific interconnected networks of brain structures, termed functional brain networks, that exhibited a predictive capacity for changes in depression scores within both treatment cohorts. These networks are illustrative of the complex organizational patterns and communication pathways between disparate regions of the brain.
More remarkably, a subset of these brain network configurations proved to be predictive of treatment response exclusively in patients receiving Yueju Pill. These predictive patterns were derived from quantitative assessments of sulcus depth and cortical thickness – anatomical features that delineate the intricate folding of the cerebral cortex and the thickness of its outermost layer, respectively. Both sulcal depth and cortical thickness are intrinsically linked to fundamental aspects of brain development, structural integrity, and functional capacity. Further granular analysis revealed that the brain’s visual processing network, in particular, played a conspicuously important role in forecasting improvements in both depressive symptoms and BDNF levels among individuals undergoing treatment with Yueju Pill.
Collectively, these groundbreaking findings strongly suggest that specific brain network signatures, discernible through high-resolution MRI scans, possess the potential to serve as reliable predictors of individual patient responses to Yueju Pill therapy for MDD. This sophisticated approach represents a significant departure from traditional symptom-based diagnostic and therapeutic paradigms, heralding a new era of personalized antidepressant care.
Should these results be substantiated through larger-scale, multi-center validation studies, this neuroimaging-guided strategy could empower clinicians with the ability to more precisely match patients to therapeutic interventions that are demonstrably more likely to yield positive outcomes, thereby substantially reducing treatment delays and enhancing overall patient recovery trajectories. As elucidated by Dr. Zhang, the principal investigator of the study, "The identified brain networks can subsequently be integrated into predictive models, such as those developed in this investigation, to forecast individual patients’ responses to Yueju Pill treatment. Based on these predicted response profiles, a determination can then be made regarding the suitability of Yueju Pill for a given patient." This pioneering research underscores the immense potential of synergistically integrating the wisdom of traditional medicinal systems with the cutting-edge capabilities of modern neuroimaging technologies, thereby paving the way for the advancement of truly precision-oriented approaches to the management of depression.