Acetaminophen, a medication found in countless homes globally, holds a unique and often underestimated position in public health. While widely regarded as a safe and effective remedy for pain and fever when used as directed, its widespread availability and the public’s perception of its benign nature conceal a far more insidious and prevalent danger: acute overdose. Contrary to popular, unsubstantiated claims circulating online about links to developmental disorders, the established and medically verified concern revolves squarely around the severe hepatotoxicity, or liver damage, that can result from exceeding recommended dosages. This well-documented risk poses a significant challenge to healthcare systems and underscores an urgent need for enhanced public awareness and advanced treatment modalities.
The scale of acetaminophen poisoning in the United States alone is staggering, positioning it as a primary driver of emergency department visits and inpatient admissions linked to over-the-counter pharmaceuticals. Each year, an estimated 56,000 individuals present to emergency departments following acetaminophen exposure beyond therapeutic levels, with approximately 2,600 requiring hospitalization for more intensive care. The implications extend far beyond initial treatment; acetaminophen toxicity is implicated in nearly half of all instances of acute liver failure observed nationally, and it accounts for a substantial 20% of all liver transplant procedures performed across the country. These figures highlight not only the immediate health crisis but also the profound long-term consequences and the considerable burden placed on organ donation and transplant services.
At the forefront of addressing this critical public health issue is a dedicated team of medical professionals and researchers. Dr. Kennon Heard, a distinguished professor within the Department of Emergency Medicine at the University of Colorado Anschutz Medical Campus and the section chief of medical toxicology, has dedicated over two and a half decades to understanding the complexities of acetaminophen poisoning. His work, alongside colleagues at institutions like CU Anschutz and Denver Health, which houses the renowned Rocky Mountain Poison & Drug Safety center, has solidified the region’s reputation as a pivotal hub for acetaminophen research. This longstanding commitment to scientific inquiry has fostered an environment where critical advancements in understanding and treating this common yet dangerous intoxication are continuously pursued.
The insidious nature of acetaminophen overdose often stems from its ubiquitous presence and the subtle ways individuals can inadvertently exceed safe limits. Acetaminophen is not only the active ingredient in widely recognized brands like Tylenol and various generic pain relievers but is also a component in a vast array of combination products targeting cold and flu symptoms, sinus congestion, and menstrual discomfort. This pervasive inclusion means that individuals may unknowingly consume multiple products containing acetaminophen simultaneously, leading to a cumulative dose that rapidly crosses the threshold of safety. The medication operates within a relatively narrow therapeutic window; while effective at prescribed doses, even slight increases can overwhelm the liver’s detoxification pathways.
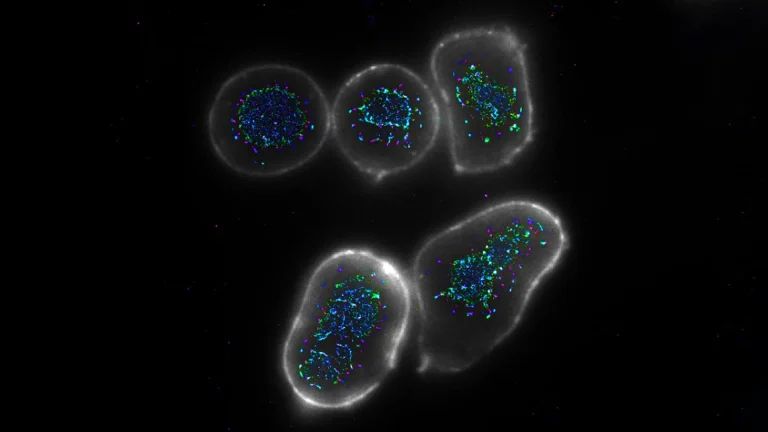
Understanding the mechanism of acetaminophen toxicity is crucial for appreciating the severity of overdose. When taken within recommended limits, acetaminophen is primarily metabolized in the liver into harmless compounds that are then excreted. However, a small fraction is converted into a highly reactive and toxic metabolite known as N-acetyl-p-benzoquinone imine, or NAPQI. Under normal circumstances, the liver’s stores of glutathione, a vital antioxidant, rapidly neutralize NAPQI. In an overdose scenario, the sheer volume of acetaminophen overwhelms the glutathione reserves, leading to an accumulation of NAPQI. This unchecked toxic metabolite then binds to liver cells, causing widespread cellular damage and necrosis, ultimately manifesting as acute liver failure.
Overdoses can arise from various circumstances, ranging from accidental ingestion to deliberate self-harm. Accidental overdoses frequently occur when individuals misunderstand dosing instructions, either by taking doses too close together, exceeding the maximum daily limit, or failing to recognize that multiple medications they are consuming all contain acetaminophen. The mindset that "more is better" can lead some to incrementally increase their dose in pursuit of greater pain relief, unknowingly pushing their liver to its limits. Another significant category involves chronic supratherapeutic ingestions, where slightly elevated doses are taken repeatedly over several days, leading to a gradual buildup of toxic metabolites and insidious liver injury that may not present acutely. Tragically, a substantial proportion of acetaminophen overdoses are also linked to intentional acts of self-harm or suicide attempts, underscoring a critical intersection with mental health crises. The accessibility of acetaminophen in nearly every household medicine cabinet makes it a readily available agent for such desperate acts.
For decades, the standard of care for acetaminophen poisoning has revolved around the administration of acetylcysteine, an effective antidote that works by replenishing the liver’s glutathione stores. When delivered promptly, ideally within eight hours of ingestion, acetylcysteine can effectively mitigate liver damage by facilitating the detoxification of NAPQI. However, a significant limitation of this treatment arises when patients present for medical attention well after this crucial therapeutic window has elapsed. As Dr. Heard points out, many individuals only seek help once they begin experiencing symptoms of liver injury, at which point the efficacy of acetylcysteine diminishes significantly, sometimes offering little to no benefit against established damage. This delay often leaves healthcare providers with limited options, highlighting the urgent need for alternative or adjunctive therapies capable of intervening effectively in later-presenting or severe cases.
In response to these challenges, pioneering research is underway to explore novel treatment strategies. Dr. Heard and his collaborators are leading a clinical trial investigating the potential of fomepizole, a medication traditionally approved for treating poisoning caused by ethylene glycol and methanol – substances commonly found in antifreeze. Fomepizole’s established mechanism involves blocking specific enzymes, known as alcohol dehydrogenases, which are responsible for converting these substances into their toxic byproducts. The idea of repurposing fomepizole for acetaminophen overdose dates back to the 1990s, when Dr. Heard was undergoing his medical toxicology training, spurred by encouraging findings from individual patient case reports and animal studies, particularly in scenarios involving severe overdoses. More recently, observations of increasing off-label use of fomepizole by clinicians for serious acetaminophen poisoning have further reinforced the rationale for formal investigation. This innovative approach gained significant momentum through the guidance of Dr. Richard Dart, a professor of emergency medicine and Dr. Heard’s longtime mentor, who has directed Rocky Mountain Poison & Drug Safety since 1992 and ultimately championed the formal testing of fomepizole in a rigorous clinical trial setting.
The ongoing phase II clinical trial is meticulously designed as a "proof of concept" study. Its primary objective is to ascertain whether the addition of fomepizole to the standard acetylcysteine regimen can effectively reduce liver damage in patients deemed at high risk following acetaminophen overdose. Participants are enrolled at multiple sites, including Denver Health, UCHealth University of Colorado Hospital, and Children’s Hospital Colorado, ensuring a diverse and representative patient pool. The study employs a randomized, double-blind methodology, meaning neither the patients nor the research team are aware of which treatment arm (fomepizole plus acetylcysteine, or acetylcysteine alone) each participant receives until the trial concludes. This rigorous design minimizes bias and enhances the reliability of the findings. Researchers will meticulously compare indicators of liver damage, primarily measured through liver enzyme levels, to determine if fomepizole confers an additional protective benefit beyond the established standard treatment. While enrollment has presented challenges due to the strict criteria required for identifying eligible high-risk patients, the team remains optimistic about enrolling approximately 40 participants within the next 12 to 18 months. Should the initial findings prove positive and demonstrate sufficient promise, the research is anticipated to advance to larger, more expansive trials. These subsequent studies would delve into longer-term patient outcomes, including overall survival rates and the necessity for liver transplantation, aiming to solidify fomepizole’s role in the future of acetaminophen overdose management.
Beyond the cutting-edge research, a crucial public health message resonates from the ongoing work of Dr. Heard and his colleagues: prevention remains paramount. Individuals are strongly advised to meticulously read and adhere to medication labels, paying close attention to recommended dosages and dosing intervals. It is imperative to be vigilant about the active ingredients in all medications consumed, especially when taking multiple products for different symptoms, as acetaminophen can often be a hidden component in various cold, flu, and pain remedies. The sobering reality, as Dr. Heard emphasizes, is that the number of fatalities stemming from accidental acetaminophen overdoses now closely rivals those resulting from intentional self-harm. This statistic underscores the urgent need for greater public awareness, responsible medication management within households, and easily accessible resources for poison control and mental health support. By fostering a deeper understanding of acetaminophen’s risks and continuing to innovate in treatment, the medical community strives to transform a prevalent danger into a manageable condition, safeguarding countless lives from this common yet perilous drug.